Welcome to our article on bicornuate vs septate uterus, where we will explore the differences between these uterine anomalies.
Understanding these conditions is essential for proper diagnosis and treatment of uterine malformations.
Whether you are experiencing symptoms or are curious about the impact on fertility and pregnancy outcomes, we’ve got you covered. Let’s dive in!
But first, let’s clarify a few terms. A bicornuate uterus and a septate uterus are both types of uterine malformations that can affect the shape and structure of the uterus.
While they may have similar symptoms and treatment options, there are distinct differences between the two.
Before we delve deeper into the details, let’s get familiar with the symptoms, diagnosis, and treatment options for both bicornuate and septate uterus.
Understanding these key aspects will help you navigate through your journey with uterine malformations.
Key Takeaways:
- Bicornuate and septate uterus are types of uterine malformations.
- Both conditions can impact fertility and pregnancy outcomes.
- Diagnosis is done through various imaging techniques.
- Treatment options include surgery and other interventions.
- Consult with a healthcare professional for personalized advice.
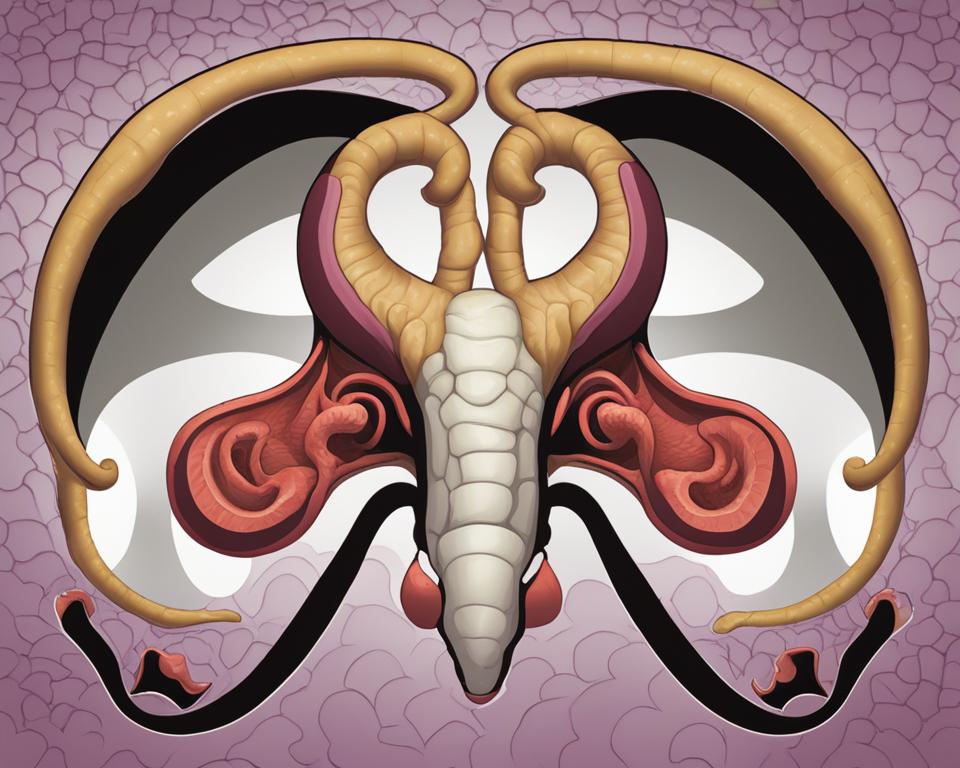
What is a Bicornuate Uterus?
A bicornuate uterus is a type of uterine malformation that occurs due to an abnormal development of the Mullerian ducts during embryogenesis. It results in a heart-shaped uterus with a large indentation on the top.
While many women with a bicornuate uterus may not experience any symptoms, others may have recurrent miscarriages, menstrual pain, and heavy bleeding.
Diagnosis of a bicornuate uterus is typically done through imaging techniques such as ultrasound, hysterosalpingography, and MRI.
These tests allow healthcare professionals to visualize the shape of the uterus and identify any abnormalities. Treatment options for a bicornuate uterus vary depending on the individual’s symptoms and fertility goals.
They may include laparoscopic surgery to correct the shape of the uterus, cervical cerclage to prevent preterm labor, and c-section for delivery.
In summary, a bicornuate uterus is a uterine malformation characterized by a heart-shaped uterus with a large indentation on the top. It can cause symptoms such as recurrent miscarriages and heavy bleeding.
Diagnosis is typically done through imaging techniques, and treatment options depend on the individual’s symptoms and fertility goals.
What is a Septate Uterus?
A septate uterus is a type of uterine malformation where a thin tissue called the septum runs down the middle of the uterus, dividing it into two separate parts.
This condition occurs due to abnormal development of the Mullerian ducts during embryogenesis.
In a complete septate uterus, the septum fully divides the uterine cavity, while in a sub septate uterus, the septum only partially divides the uterus.
Women with a septate uterus may experience symptoms such as recurrent miscarriages, preterm labor, and reproductive complications.Diagnosing a septate uterus can be done through various methods.
A pelvic exam can reveal the presence of a uterine anomaly, and imaging techniques like transvaginal ultrasonography and MRI can provide detailed visualization of the uterus and the septum.
Additionally, a hysteroscopy may be performed to directly visualize the uterine cavity and confirm the presence of the septum.
Treatment options for a septate uterus include hysteroscopic metroplasty, which involves removing the septum to restore a normal uterine cavity.
This procedure can be performed using minimally invasive techniques, minimizing the risk and recovery time for patients.
By removing the dividing septum, the uterus becomes more conducive to successful pregnancies, reducing the likelihood of complications and miscarriages.
| Septate Uterus | Bicornuate Uterus | |
|---|---|---|
| Definition | A uterine malformation where a septum divides the uterus | A uterine malformation with a heart-shaped external shape and a large indentation on the top |
| Shape | Normal external shape with a dividing septum inside | Heart-shaped external shape with a large indentation on the top |
| Impact on Pregnancy | Increased risk of miscarriage, preterm labor, and reproductive complications | Increased risk of miscarriage and preterm labor |
| Diagnosis | Pelvic exam, transvaginal ultrasonography, MRI, hysteroscopy | Pelvic exam, ultrasound, hysterosalpingography, MRI |
| Treatment | Hysteroscopic metroplasty to remove the septum | Laparoscopic surgery, cervical cerclage, c-section |
Similarities Between Bicornuate and Septate Uterus
When it comes to uterine malformations, bicornuate and septate uterus share several similarities.
Both conditions are categorized as Mullerian duct anomalies, resulting from abnormal development of the reproductive tract during embryogenesis.
This can lead to structural abnormalities in the uterus, affecting fertility and pregnancy outcomes.
While the specific shapes of the uterus differ between the two conditions, the diagnostic methods for bicornuate and septate uterus are similar.
Healthcare professionals utilize imaging techniques such as ultrasound, MRI, and hysteroscopy to visualize the uterine cavity and identify any abnormalities. These methods allow for accurate diagnosis and appropriate treatment planning.
Speaking of treatment options, both bicornuate and septate uterus can be addressed through surgical interventions.
Laparoscopic surgery and hysteroscopic metroplasty are commonly performed procedures to correct the structural abnormalities associated with these conditions.
Additionally, cervical cerclage may be recommended to prevent pregnancy complications in certain cases.
Overall, understanding the similarities between bicornuate and septate uterus is essential for healthcare professionals to provide accurate diagnoses and appropriate treatment plans.
By utilizing similar diagnostic methods and treatment options, they can effectively address the unique challenges posed by these uterine malformations.
Table: Similarities Between Bicornuate and Septate Uterus
| Bicornuate Uterus | Septate Uterus |
|---|---|
| Mullerian duct anomaly | Mullerian duct anomaly |
| Affects fertility and pregnancy outcomes | Affects fertility and pregnancy outcomes |
| Diagnostic methods: ultrasound, MRI, hysteroscopy | Diagnostic methods: ultrasound, MRI, hysteroscopy |
| Treatment options: laparoscopic surgery, hysteroscopic metroplasty, cervical cerclage | Treatment options: laparoscopic surgery, hysteroscopic metroplasty, cervical cerclage |
Differences Between Bicornuate and Septate Uterus
When comparing bicornuate and septate uterus, the key differences lie in the shape of the uterus and the presence of a dividing septum.
A bicornuate uterus has a heart-shaped external shape with an indentation on the top, resembling the shape of a “V.” On the other hand, a septate uterus has a normal external shape, with a dividing septum inside that separates the uterus into two separate parts.
These differences in shape can have implications on fertility, pregnancy outcomes, and the symptoms experienced by individuals with these uterine malformations.
While both conditions can lead to recurrent miscarriages and reproductive complications, the presence of a dividing septum in a septate uterus may increase the risk further.
Diagnosing the specific type of uterine malformation is important for developing an appropriate treatment plan.
Pelvic exams, ultrasound, MRI, and hysteroscopy are common diagnostic methods used to identify and differentiate between a bicornuate and septate uterus.
Treatment options may include laparoscopic surgery, hysteroscopic metroplasty, cervical cerclage, or other interventions depending on the individual’s circumstances.
Table: Comparing Bicornuate and Septate Uterus
| Aspect | Bicornuate Uterus | Septate Uterus |
|---|---|---|
| Shape of Uterus | Heart-shaped, resembling a “V” with an indentation on the top | Normal shape with a dividing septum inside |
| Severity of Symptoms | Symptoms may vary; some individuals may be asymptomatic | Risk of recurrent miscarriages and reproductive complications may be higher |
| Diagnostic Methods | Pelvic exams, ultrasound, MRI, hysteroscopy | Pelvic exams, ultrasound, MRI, hysteroscopy |
| Treatment Options | Laparoscopic surgery, cervical cerclage, c-section | Hysteroscopic metroplasty, surgical removal of the septum |
Understanding the differences between bicornuate and septate uterus is vital for healthcare professionals in providing appropriate care and treatment for individuals with these uterine malformations.
Each condition presents its unique challenges, and by recognizing these distinctions, healthcare providers can tailor treatment plans to address the specific needs of their patients.
Diagnostic Methods and Treatment Options
When it comes to diagnosing and treating bicornuate and septate uterus, healthcare professionals have a range of options at their disposal.
These uterine malformations can be identified through various imaging techniques, such as pelvic exams, ultrasound, MRI, and hysteroscopy.
These methods allow for a clear visualization of the shape of the uterus and any abnormalities present.
Once a diagnosis has been made, treatment options can be explored. For both bicornuate and septate uterus, surgical procedures are commonly used.
Laparoscopic surgery is often employed to correct abnormalities and reshape the uterus, while hysteroscopic metroplasty can be performed to remove the dividing septum in cases of a septate uterus.
Additionally, cervical cerclage may be recommended to prevent complications during pregnancy.
It is important to note that the choice of treatment will depend on the specific condition and the individual needs of the patient.
A healthcare professional will consider factors such as the severity of the malformation, the patient’s fertility goals, and any associated symptoms.
Therefore, it is crucial for each case to be assessed on an individual basis to determine the most appropriate course of action.
In summary, diagnostic methods for bicornuate and septate uterus include pelvic exams, ultrasound, MRI, and hysteroscopy.
These imaging techniques allow for a thorough evaluation of the uterus and aid in the identification of any abnormalities.
Treatment options typically involve surgical procedures such as laparoscopic surgery, hysteroscopic metroplasty, and cervical cerclage.
The choice of treatment will depend on the individual needs and circumstances of the patient. Consulting with a healthcare professional is essential in order to determine the most suitable approach for each specific case.
FAQ
What are the symptoms of a bicornuate uterus?
Symptoms of a bicornuate uterus may include recurrent miscarriages, menstrual pain, and heavy bleeding.
What are the symptoms of a septate uterus?
Symptoms of a septate uterus may include recurrent miscarriages, preterm labor, and reproductive complications.
How are bicornuate and septate uterus diagnosed?
Bicornuate and septate uterus can be diagnosed through pelvic exams, ultrasound, MRI, and hysteroscopy.
What are the treatment options for a bicornuate uterus?
Treatment options for a bicornuate uterus include laparoscopic surgery, cervical cerclage, and c-section.
What are the treatment options for a septate uterus?
Treatment options for a septate uterus include hysteroscopic metroplasty, which involves removing the septum.
What is the main difference between a bicornuate uterus and a septate uterus?
The main difference is in the shape of the uterus and the presence of a dividing septum in the case of a septate uterus.
How can uterine malformations affect fertility and pregnancy outcomes?
Uterine malformations can impact fertility and pregnancy outcomes, but with proper diagnosis and treatment, many women can achieve successful pregnancies.
What should I do if I suspect I have a bicornuate or septate uterus?
If you suspect you have a bicornuate or septate uterus, it is important to consult with a healthcare professional for proper diagnosis and guidance on the best treatment options for your individual circumstances.
Conclusion
In conclusion, understanding the differences between a bicornuate uterus and a septate uterus is essential when dealing with uterine malformations.
Both conditions are caused by abnormalities in the development of the Mullerian ducts and can impact fertility and pregnancy outcomes.
However, with the right diagnosis and treatment options, women with these uterine malformations can still have successful pregnancies.
It is important to consult with a healthcare professional to determine the best course of action based on individual circumstances.
By utilizing imaging techniques such as ultrasound, MRI, and hysteroscopy, healthcare professionals can accurately diagnose bicornuate and septate uteruses.
Treatment options may include surgical procedures like laparoscopic surgery, hysteroscopic metroplasty, and cervical cerclage, depending on the specific condition and the needs of the patient.
Overall, with advancements in medical technology and expert care, women with bicornuate or septate uteruses can have a comprehensive understanding of their condition and access to various treatment options to improve fertility and achieve positive pregnancy outcomes.
![Ray Dalio Quotes [Principles, Life, Investment]](https://tagvault.org/wp-content/uploads/2023/04/Screen-Shot-2023-04-19-at-7.57.49-PM.png)
