Welcome to our comprehensive guide on caseating and non caseating granulomas. In the world of medical terminology, these terms often come up when discussing granulomas and their implications. Whether you’re a healthcare professional or someone curious about this topic, this article will provide you with a clear understanding of caseating and non caseating granulomas and their significance.
Key Takeaways:
- Granulomas are small areas of chronic inflammation characterized by a collection of macrophages.
- Caseating granulomas have a central region of necrosis and appear “cheese-like” upon biopsy.
- Noncaseating granulomas do not have a central region of necrosis.
- Granulomas can be formed in response to infections, inflammatory conditions, and exposure to foreign objects.
- Understanding the differences between caseating and non caseating granuloma is important for proper diagnosis and treatment of granulomatous diseases.
What is a Granuloma?
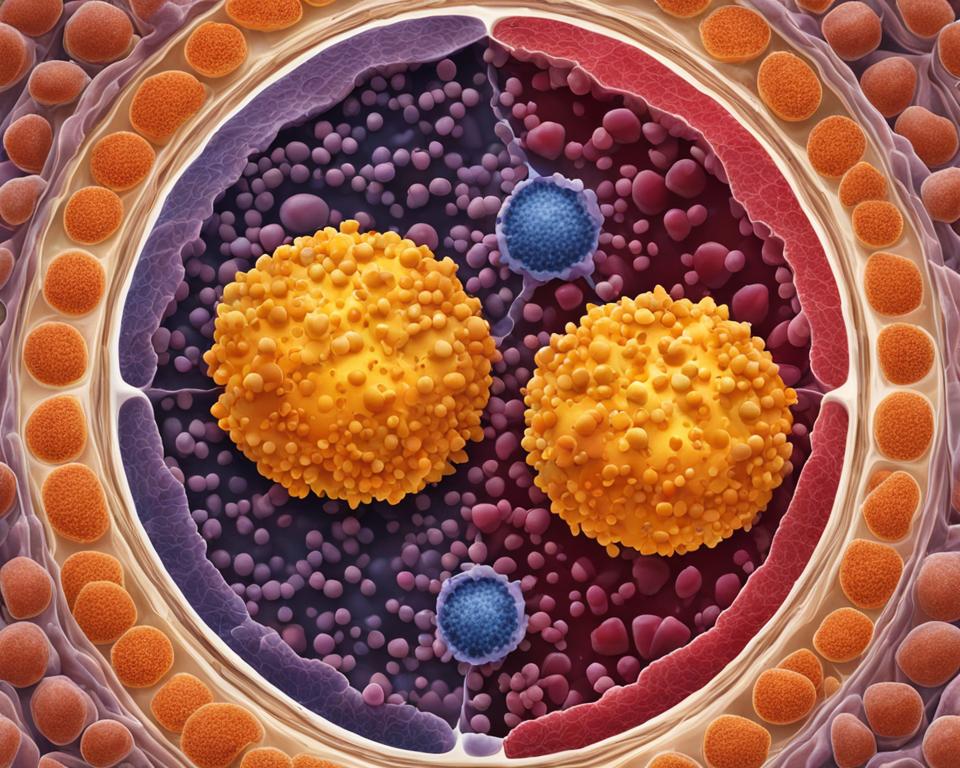
A granuloma is a small area of chronic inflammation characterized by a collection of macrophages. These specialized white blood cells play a crucial role in the immune response by engulfing and killing foreign substances. Granulomas can form in various parts of the body and are a defense mechanism employed by the immune system to protect against invading pathogens.
One of the key players in granuloma formation is the T-cell, specifically the TH1 subtype. When an infection or foreign object is present, antigen-presenting cells, such as macrophages, present the foreign antigen to CD4+ helper T-cells. This interaction activates the T-cells, leading to the secretion of cytokines and the conversion of CD4+ helper T-cells to the TH1 subtype. TH1 cells then accumulate at the site of inflammation and secrete additional cytokines and chemokines, resulting in the accumulation of inflammatory cells and the formation of a granuloma.
Granulomas are a fascinating aspect of the immune response and play a critical role in protecting the body from harmful pathogens. By understanding the mechanisms behind granuloma formation, researchers and healthcare professionals can better diagnose and treat granulomatous diseases.
Types of Granulomas
A granuloma is a small area of chronic inflammation characterized by a collection of macrophages. These granulomas can be classified into different types based on their characteristics and underlying causes.
Caseating Granuloma
A caseating granuloma is characterized by a central region of necrosis, giving it a “cheese-like” appearance. This type of granuloma usually forms in response to certain infections, such as tuberculosis and fungal infections. The necrotic center is surrounded by a rim of activated macrophages, lymphocytes, and fibroblasts. In tuberculosis, the central necrosis is caused by the immune response attempting to contain the infection.
Noncaseating Granuloma
A noncaseating granuloma, on the other hand, does not have a central region of necrosis. It is typically formed in response to conditions such as sarcoidosis, Crohn’s disease, and exposure to foreign materials. The absence of necrosis in these granulomas suggests a different underlying mechanism of formation. Noncaseating granulomas are composed of activated macrophages, epithelioid cells, and lymphocytes.
Foreign Body Granuloma
In addition to caseating and noncaseating granulomas, there is also a type known as foreign body granuloma. This type of granuloma is formed in response to the presence of foreign objects in the body, such as surgical implants or non-absorbable sutures. The body’s immune response attempts to encapsulate and isolate the foreign material, resulting in the formation of granulomas around it.
Understanding the different types of granulomas is crucial for diagnosing and treating granulomatous diseases. The specific type of granuloma observed can provide valuable information about the underlying cause and guide appropriate management strategies.
| Granuloma Type | Characteristics | Underlying Causes |
|---|---|---|
| Caseating Granuloma | Central necrosis, “cheese-like” appearance | Tuberculosis, fungal infections |
| Noncaseating Granuloma | No central necrosis | Sarcoidosis, Crohn’s disease, foreign material exposure |
| Foreign Body Granuloma | Formed around foreign objects | Surgical implants, non-absorbable sutures |
Causes of Granulomas
Granulomas are a result of chronic inflammation and can be caused by various factors. The most common causes of granulomas are infections, including tuberculosis and fungal infections. In these cases, the body’s immune response leads to the formation of granulomas as a way to contain and fight off the invading pathogens.
In addition to infections, granulomas can also be caused by inflammatory conditions such as sarcoidosis and Crohn’s disease. These conditions trigger an ongoing immune response, leading to the formation of granulomas. Granulomas can also occur in vasculitis, which is a condition characterized by inflammation of blood vessels. Exposure to foreign objects can also trigger the formation of granulomas as the body tries to protect itself from the presence of these foreign substances.
Chronic inflammation, infections, inflammatory conditions, vasculitis, and exposure to foreign objects are some of the common causes of granulomas.Granulomas can occur in various parts of the body, including the lungs, liver, skin, and lymph nodes.
It is important to identify the cause of the granulomas to determine the appropriate treatment approach. Infections may require antimicrobial medications, while inflammatory conditions may necessitate anti-inflammatory drugs. In some cases, surgical intervention may be needed to remove foreign objects or tissue that is causing the granulomas. Addressing the underlying cause is crucial for managing and resolving granulomatous diseases.
Table: Common Causes of Granulomas
| Causes | Description |
|---|---|
| Infections | Includes tuberculosis and fungal infections |
| Inflammatory Conditions | Sarcoidosis, Crohn’s disease |
| Vasculitis | Inflammation of blood vessels |
| Exposure to Foreign Objects | Foreign body granulomas |
Understanding the causes of granulomas is crucial for accurately diagnosing and treating these conditions. By addressing the underlying factors and providing appropriate medical intervention, healthcare professionals can help manage and alleviate the symptoms associated with granulomatous diseases.
Formation of Granulomas
Granulomas form as a result of the immune system’s response to various causative agents, such as infections and foreign objects. The process begins with the activation of antigen presenting cells, primarily macrophages, which present the foreign antigens to CD4+ helper T-cells. This interaction triggers T-cell activation and the secretion of cytokines, which ultimately leads to the conversion of CD4+ helper T-cells into the TH1 subtype.
The accumulation of TH1 cells in the affected area, along with the continuous secretion of cytokines and chemokines, creates an environment conducive to the formation of granulomas. Inflammatory cells, including macrophages, lymphocytes, and epithelioid cells, accumulate, resulting in the characteristic appearance of the granuloma.
This immune response and the subsequent formation of granulomas serve as a protective mechanism for the body. By encapsulating and surrounding the causative agent, the granuloma helps to prevent the spread of infection and limits the damage caused by foreign objects.
Key Steps in Granuloma Formation:
- Antigen presenting cells, such as macrophages, present foreign antigens to CD4+ helper T-cells.
- CD4+ helper T-cells are activated and secrete cytokines.
- Cytokines induce the conversion of CD4+ helper T-cells into TH1 cells.
- TH1 cells accumulate and secrete cytokines and chemokines.
- Inflammatory cells, including macrophages, lymphocytes, and epithelioid cells, accumulate, leading to granuloma formation.
This intricate immune system response plays a crucial role in the development of granulomas and helps to protect the body from various harmful agents.
Diagnosis and Treatment of Granulomas
Diagnosing granulomas involves a comprehensive approach that includes medical examination, imaging tests, biopsy, and blood tests. These diagnostic methods help to confirm the presence of granulomas, identify the underlying cause, and guide appropriate treatment options.
Imaging: Imaging tests such as X-rays, computed tomography (CT) scans, or magnetic resonance imaging (MRI) can be used to visualize the presence of granulomas in specific areas of the body. These tests provide valuable information about the size, location, and distribution of the granulomas, aiding in the diagnosis and treatment planning.
Biopsy: A biopsy involves the removal of a small tissue sample from the affected area for microscopic examination. It helps to determine whether the granuloma is caseating or noncaseating and provides insights into the underlying cause. Biopsies can be performed using various methods, including needle aspiration, excisional biopsy, or endoscopic procedures.
Blood tests: Blood tests may be conducted to evaluate specific biomarkers associated with different causes of granulomas. For example, tests for tuberculosis, sarcoidosis, or autoimmune diseases can help identify the underlying condition contributing to the granuloma formation. Blood tests can also assess inflammatory markers and immune system function, aiding in the overall diagnosis and management of granulomatous diseases.
“Accurate diagnosis of granulomas is crucial for effective treatment and management. A multidisciplinary approach involving radiologists, pathologists, and other healthcare professionals is often required to ensure a comprehensive evaluation and appropriate treatment plan for granuloma patients.”
Treatment of granulomas primarily depends on the underlying cause and the severity of symptoms. In some cases, granulomas may not require active treatment as they can resolve on their own. However, when treatment is necessary, it aims to reduce inflammation, manage symptoms, and address the underlying condition contributing to granuloma formation.
Treatment options may include:
- Medications: Anti-inflammatory drugs, immunosuppressive agents, or corticosteroids may be prescribed to reduce inflammation and regulate the immune response.
- Antibiotics: In the case of granulomas caused by infections, appropriate antibiotics targeting the specific pathogen may be prescribed to control the infection and prevent further granuloma formation.
- Surgical intervention: In certain situations, surgical removal of the granulomas or the underlying cause may be necessary, especially when they lead to complications or cause significant organ damage.
- Management of underlying conditions: Granulomas associated with chronic diseases such as sarcoidosis or Crohn’s disease may require targeted treatment to manage the underlying condition and prevent further granuloma formation.
It is essential for individuals with granulomas to receive ongoing medical care and follow-up to monitor their condition, evaluate treatment effectiveness, and address any potential complications. Regular check-ups and close collaboration with healthcare professionals are vital to managing granulomatous diseases effectively.
Granulomas and Their Prognosis
When it comes to the prognosis of granulomas, it largely depends on the underlying cause. Some granulomas may regress on their own, while others may require treatment to fully resolve. The regression of granulomas can vary based on factors such as the severity of the underlying condition and the effectiveness of the chosen treatment.
For example, granuloma annulare, a skin condition characterized by the formation of small, ring-shaped bumps, often spontaneously regresses without treatment. On the other hand, granulomas caused by tuberculosis require treatment with appropriate medication to eliminate the infection and facilitate the regression of the granulomas.
It’s important to note that the presence of granulomas can also indicate certain disease conditions, and the prognosis may be influenced accordingly. For instance, in cases where granulomas are associated with an autoimmune disease like sarcoidosis or granulomatosis with polyangiitis (GPA), the overall prognosis will depend on the management of the underlying disease and the response to treatment.
“The regression of granulomas can vary based on factors such as the severity of the underlying condition and the effectiveness of the chosen treatment.”
| Underlying Cause | Prognosis |
|---|---|
| Tuberculosis | Requires treatment with medication for regression |
| Granuloma annulare | May regress spontaneously without treatment |
| Autoimmune diseases (e.g., sarcoidosis, GPA) | Prognosis depends on management and response to treatment of the underlying disease |
Understanding the underlying cause of granulomas and closely monitoring their regression is crucial for appropriate management and obtaining the best possible outcome for patients.
Conclusion
In conclusion, granulomas are small areas of chronic inflammation characterized by a collection of macrophages. Understanding the differences between caseating and noncaseating granulomas is essential for proper diagnosis and treatment of granulomatous diseases.
Caseating granulomas, with a central region of necrosis, are often caused by infections such as tuberculosis and fungal infections. On the other hand, noncaseating granulomas, without necrosis, can be caused by inflammatory conditions like sarcoidosis and Crohn’s disease, as well as exposure to foreign objects.
The formation, diagnosis, and treatment of granulomas depend on the underlying cause. Medical examination, imaging, biopsy, and blood tests are used to diagnose granulomas, and treatment involves targeting the underlying inflammation. Medications like anti-TNF therapy are commonly used, and additional treatments may be necessary depending on the specific cause.
Overall, recognizing the characteristics of caseating and noncaseating granulomas plays a crucial role in managing granulomatous diseases effectively. By identifying the type of granuloma and its underlying cause, healthcare professionals can provide appropriate treatment and improve patient outcomes.
FAQ
What is a granuloma?
A granuloma is a small area of chronic inflammation characterized by a collection of macrophages.
What are the types of granulomas?
There are two types of granulomas: caseating and noncaseating. Caseating granulomas have a central region of necrosis, while noncaseating granulomas do not.
What causes granulomas?
Granulomas can be formed in response to infections, inflammatory conditions, and exposure to foreign objects.
How are granulomas formed?
Granulomas form when the immune system responds to causative agents such as infections and foreign objects.
How are granulomas diagnosed and treated?
Granulomas can be diagnosed through medical examination, imaging, biopsy, and blood tests. Treatment involves medications that target underlying inflammation.
What is the prognosis of granulomas?
The prognosis of granulomas depends on the underlying cause. Some granulomas may go away on their own, while others may require treatment.