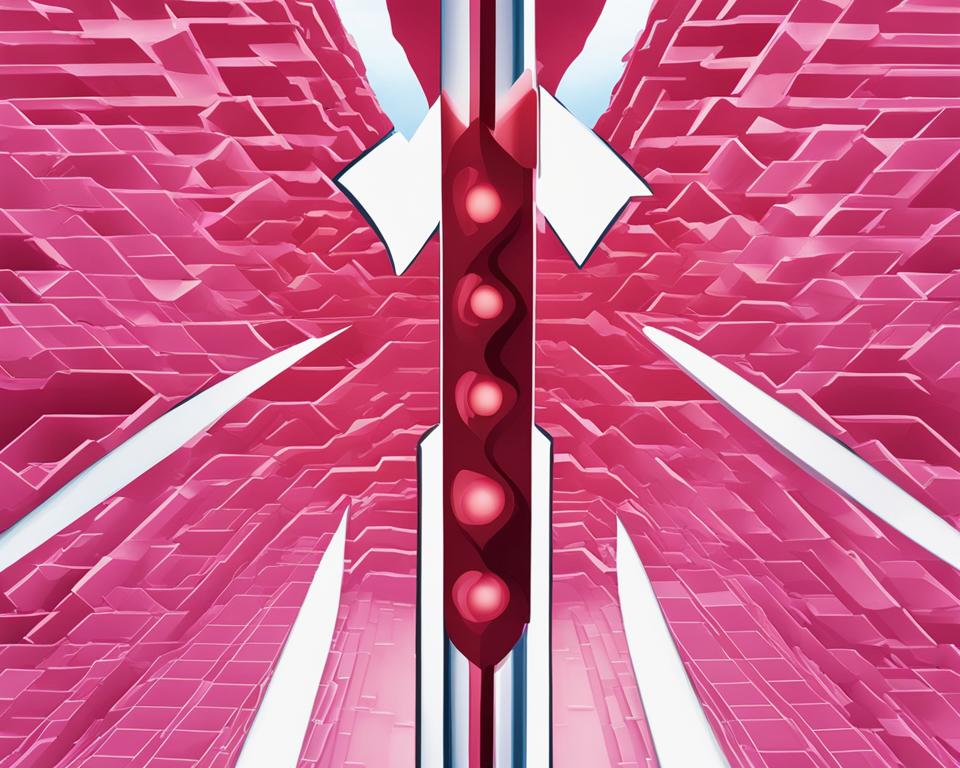
Welcome to our article where we will explore and explain the key differences between diverticulitis and diverticulosis. These two conditions may sound similar, but they have distinct characteristics, seriousness, and treatment approaches. Understanding the disparities between diverticulitis and diverticulosis is crucial for proper diagnosis, treatment, and prevention. Let’s dive in!
Key Takeaways:
- Diverticulosis and diverticulitis are two separate conditions involving the development of pouches in the colon wall.
- Diverticulosis is usually asymptomatic, while diverticulitis causes abdominal pain and can lead to complications.
- The exact cause of diverticulosis is unknown, but factors such as a low-fiber diet and sedentary lifestyle may increase the risk.
- Diagnosing diverticulosis and diverticulitis often requires imaging tests like colonoscopy or CT scan.
- Treatment options range from dietary changes and antibiotics to hospitalization and surgical interventions.
Symptoms and Diagnosis of Diverticulosis and Diverticulitis
Diverticulosis and diverticulitis have distinct symptoms and require different diagnostic approaches. While diverticulosis often does not cause symptoms, it can lead to chronic issues such as bloating, constipation, diarrhea, or abdominal pain. On the other hand, diverticulitis presents with sudden and severe abdominal symptoms, including intense abdominal pain, fever, chills, nausea, vomiting, constipation, or diarrhea. In some cases, diverticula can bleed, resulting in rectal bleeding or bloody stool. Recognizing these symptoms is crucial for accurate diagnosis and timely treatment.
To diagnose diverticulosis and diverticulitis, healthcare professionals may use various imaging tests such as colonoscopy or CT scan. These tests allow for a detailed examination of the colon and identification of diverticula, inflammation, or infection. Additionally, blood work and stool samples may be taken to rule out other conditions and assess the severity of diverticulitis. It is important to consult a medical professional for an accurate diagnosis and appropriate treatment plan.
“I experienced intense abdominal pain and was diagnosed with diverticulitis. It was essential to undergo a colonoscopy to confirm the diagnosis and assess the extent of the inflammation. The imaging tests provided valuable insights into the condition and helped guide the treatment plan.” – Patient Testimonial
Causes of Diverticulosis and Diverticulitis
The causes of diverticulosis and diverticulitis are not yet fully understood. However, certain risk factors have been identified. Diverticulosis is more commonly observed in individuals over the age of 40 and is associated with a low-fiber diet, sedentary lifestyle, and obesity. These factors contribute to increased pressure within the colon, leading to the formation of diverticula. On the other hand, diverticulitis can occur when the diverticula become blocked with fecal matter, allowing bacteria to grow and cause inflammation or infection. Understanding these underlying causes can help in the management and prevention of diverticular diseases.
| Diverticulosis | Diverticulitis | |
|---|---|---|
| Common Symptoms | Bloating, constipation, diarrhea, mild abdominal pain | Intense abdominal pain, fever, chills, nausea, vomiting, constipation, diarrhea |
| Diagnostic Tests | Colonoscopy, CT scan, blood work, stool samples | Colonoscopy, CT scan, blood work, stool samples |
| Underlying Causes | Low-fiber diet, sedentary lifestyle, obesity | Blockage of diverticula by fecal matter, bacterial infection |
Treatment and Management of Diverticulosis and Diverticulitis
When it comes to the treatment and management of diverticulosis and diverticulitis, the approach varies based on the severity of the condition. For individuals with diverticulosis that does not cause symptoms, treatment may not be necessary. However, dietary changes are often recommended to prevent complications. Increasing fiber intake and consuming probiotic-rich foods can help promote healthy digestion and prevent the development of diverticulitis.
On the other hand, diverticulitis requires treatment to alleviate symptoms and prevent further complications. Mild cases can usually be managed with antibiotics to clear the infection. In addition, a liquid diet may be recommended initially, followed by a gradual reintroduction of solid foods. This allows the inflamed pouches in the colon to heal and reduces strain on the digestive system.
In more severe cases of diverticulitis or when complications arise, hospitalization may be necessary. Intravenous antibiotics may be administered to treat the infection, and procedures such as drainage of abscesses or surgery may be required. These interventions aim to resolve the infection, remove any blockages or abscesses, and prevent the need for further emergency intervention.
| Treatment Approach | Diverticulosis | Diverticulitis |
|---|---|---|
| Dietary Changes | Increased fiber intake | Liquid diet, gradual reintroduction of solid foods |
| Medication | N/A | Antibiotics to clear infection |
| Procedures | N/A | Drainage of abscesses, surgery if necessary |
It is important for individuals with diverticulosis or diverticulitis to closely follow their healthcare provider’s recommendations and attend regular check-ups. By doing so, they can monitor their condition, track any changes, and ensure timely treatment if needed. Engaging in healthy lifestyle habits, such as maintaining a healthy weight, quitting smoking, and exercising regularly, can also contribute to the management and prevention of diverticular diseases.
Prevention of Diverticulosis and Diverticulitis
Preventing diverticulosis and diverticulitis involves making certain lifestyle changes to reduce the risk of developing these conditions. By adopting healthy habits, individuals can potentially minimize their chances of experiencing symptoms and complications associated with diverticular diseases.
Eating a High-Fiber Diet
One of the key preventive measures is maintaining a high-fiber diet. Consuming an adequate amount of fiber can help promote regular bowel movements and prevent the formation of diverticula. Foods rich in fiber include fruits, vegetables, whole grains, beans, and legumes. It is recommended to gradually increase fiber intake to avoid digestive discomfort.
Maintaining a Healthy Weight and Regular Exercise
Another important aspect of prevention is maintaining a healthy weight and engaging in regular physical activity. Obesity and a sedentary lifestyle have been linked to an increased risk of diverticular diseases. By managing weight and staying active, individuals can support overall digestive health and reduce the likelihood of developing diverticula and experiencing subsequent complications.
Quitting Smoking and Avoiding Excessive NSAID Use
Smoking has been associated with an increased risk of diverticulitis, so quitting smoking is highly recommended for prevention. Additionally, minimizing the use of nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or aspirin, can help reduce the risk of diverticular diseases. If pain relief is needed, alternative options or consult with a healthcare professional should be considered.
Conclusion
In conclusion, understanding the difference between diverticulitis and diverticulosis is key to managing these conditions effectively. Diverticulosis, characterized by the development of small pouches in the colon wall, is a common and often asymptomatic condition. On the other hand, diverticulitis occurs when these pouches become inflamed or infected, causing abdominal pain and potential complications.
Diagnosing diverticulosis and diverticulitis involves various imaging tests, such as colonoscopy or CT scan, along with blood work and stool samples. Treatment options for diverticulosis usually involve dietary changes, while diverticulitis may require antibiotics, a liquid diet, or even surgical interventions in severe cases.
Prevention strategies for diverticulosis and diverticulitis include maintaining a healthy weight, adopting a high-fiber diet, and avoiding risk factors such as smoking and excessive use of NSAIDs. Regular medical check-ups and early detection are crucial in preventing complications and ensuring timely treatment.
By being aware of the symptoms, understanding the risks, and taking proactive steps towards prevention, individuals can effectively manage diverticular diseases and maintain their overall gastrointestinal health.
FAQ
What is diverticulosis?
Diverticulosis is the development of small pouches in the colon wall. It is a common condition that often goes unnoticed and does not typically cause symptoms.
What is diverticulitis?
Diverticulitis occurs when the pouches in the colon wall become inflamed or infected. It causes abdominal pain and can lead to complications.
What are the symptoms of diverticulosis?
Diverticulosis typically does not cause symptoms, but it can lead to chronic problems such as bloating, constipation, diarrhea, or abdominal pain.
What are the symptoms of diverticulitis?
Diverticulitis causes sudden and severe abdominal symptoms, including intense abdominal pain, fever, chills, nausea, vomiting, constipation, or diarrhea. In some cases, diverticula can bleed, resulting in rectal bleeding or bloody stool.
How is diverticulosis and diverticulitis diagnosed?
Diagnosing diverticulosis and diverticulitis often involves imaging tests such as colonoscopy or CT scan. Blood work and stool samples may also be taken to rule out other conditions.
What is the treatment for diverticulosis?
Treatment for diverticulosis usually involves dietary changes, such as increasing fiber intake and consuming probiotic-rich foods. In most cases, no treatment is needed if diverticulosis does not cause symptoms.
How is diverticulitis treated?
Mild cases of diverticulitis can be managed with antibiotics to clear the infection, along with a liquid diet initially, followed by a gradual reintroduction of solid foods. Severe cases or complications may require hospitalization, where patients receive intravenous antibiotics and may undergo drainage of abscesses or surgery.
Can diverticulosis and diverticulitis be prevented?
While diverticulosis and diverticulitis cannot always be prevented, certain lifestyle changes can help reduce the risk. Maintaining a healthy weight, quitting smoking, and exercising regularly are recommended. Eating a high-fiber diet and reducing red meat intake may also lower the risk of diverticulitis.
What should I do if I experience symptoms of diverticulitis?
It is important to be aware of the symptoms of diverticulitis or diverticular bleeding. If you experience intense abdominal pain, fever, chills, nausea, vomiting, constipation, diarrhea, rectal bleeding, or bloody stool, you should seek immediate medical attention.