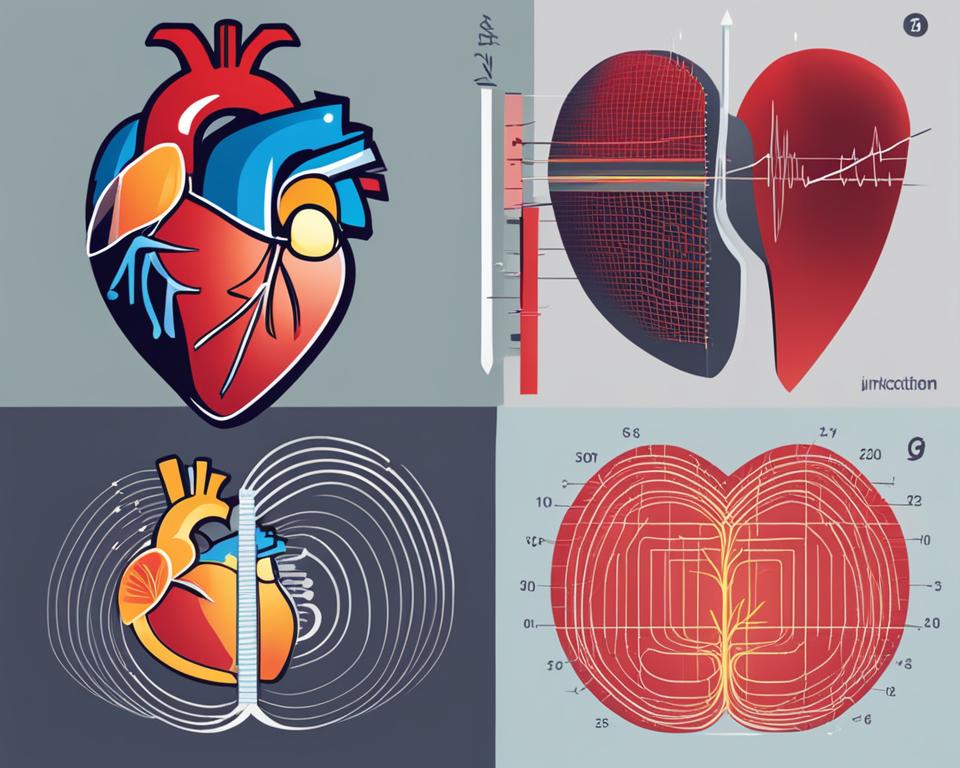
Welcome to our article on idioventricular rhythm vs junctional rhythm, two types of cardiac arrhythmias that fall under heart rhythm disorders. These rhythm abnormalities occur due to dysfunctions in the heart conduction system, specifically the ventricular rhythm and atrioventricular junction. Understanding the differences between these two rhythms is crucial for accurate EKG interpretation and proper management of rhythm abnormalities.
Key Takeaways:
- Idioventricular rhythm and junctional rhythm are types of cardiac arrhythmias that arise from abnormalities in the heart conduction system.
- Idioventricular rhythm is characterized by a slow regular ventricular rhythm, while junctional rhythm occurs when the atrioventricular junction acts as the pacemaker.
- EKG interpretation plays a crucial role in diagnosing and distinguishing between these two rhythms.
- Sinus node dysfunction is one of the causes of rhythm abnormalities.
- Proper management and treatment options for idioventricular rhythm and junctional rhythm depend on the underlying causes and severity of symptoms.
In the following sections, we will delve deeper into the characteristics, similarities, differences, evaluation, diagnosis, and management of idioventricular rhythm and junctional rhythm. Let’s explore these rhythm abnormalities further to enhance our understanding and improve patient care.
Characteristics of Idioventricular Rhythm
Idioventricular rhythm, also known as slow ventricular tachycardia, is characterized by a slow regular ventricular rhythm with a rate of less than 50 bpm. This rhythm can also be observed as accelerated idioventricular rhythm when the rate ranges between 50 to 100 bpm. The absence of P waves and a prolonged QRS interval are key features of idioventricular rhythm. It is important to note that idioventricular rhythm is commonly observed in various conditions, including AV block, myocardial infarction, electrolyte imbalances, certain medications, and congenital heart diseases. In addition, athletes may experience idioventricular rhythm due to a decrease in sympathetic tone during intense physical activities.
| Characteristic | Description |
|---|---|
| Rate | Less than 50 bpm (slow ventricular tachycardia) |
| QRS Complex | Prolonged |
| P Waves | Absent |
| Etiology | AV block, myocardial infarction, electrolyte imbalances, certain medications, congenital heart diseases |
| Sports-related Influences | Decreased sympathetic tone during intense physical activity |
Recognizing the characteristic features and understanding the etiologies associated with idioventricular rhythm is crucial for proper evaluation and management. Identifying and addressing the underlying causes are essential steps in developing an appropriate treatment plan. It is important to note that idioventricular rhythm is generally considered a benign rhythm unless accompanied by symptoms or associated with other significant cardiac issues. Therefore, close monitoring and regular follow-up assessments are key in managing patients with idioventricular rhythm.
“Idioventricular rhythm is characterized by a slow regular ventricular rhythm with a rate of less than 50 bpm. It can occur in various conditions, including AV block, myocardial infarction, electrolyte imbalances, certain medications, and congenital heart diseases. Recognition of its characteristic features and associated etiologies is essential for accurate evaluation and management.”
Characteristics of Junctional Rhythm
Junctional rhythm is an abnormal heart rhythm that occurs when the atrioventricular (AV) junction, specifically the AV node, acts as the pacemaker in the absence of normal sinus rhythm. It is diagnosed on an ECG by the absence of P waves or the presence of inverted P waves. Understanding the characteristics of junctional rhythm is crucial for accurate diagnosis and treatment.
Causes
Junctional rhythm can be caused by various factors, including SA node dysfunction, AV block, myocardial ischemia, and certain medications. SA node dysfunction refers to the impairment of the sinoatrial (SA) node, the natural pacemaker of the heart, which can lead to the AV junction taking over as the pacemaker. AV block occurs when the electrical signals between the atria and ventricles are delayed or blocked. Myocardial ischemia, which is a lack of blood and oxygen supply to the heart muscle, can also disrupt the normal conduction system. Additionally, certain medications, such as beta-blockers or calcium channel blockers, can affect the AV node and contribute to the development of junctional rhythm.
Symptoms and Diagnosis
The symptoms of junctional rhythm can vary depending on the underlying cause and individual patient. Some common symptoms include palpitations (rapid or irregular heartbeat), lightheadedness, fatigue, and syncope (fainting). To diagnose junctional rhythm, an electrocardiogram (ECG) is performed to assess the heart’s electrical activity. The absence of P waves or the presence of inverted P waves on the ECG is a characteristic finding of junctional rhythm.
Treatment Options
The treatment of junctional rhythm depends on the severity of symptoms and the underlying cause. In some cases, no specific treatment may be required if the rhythm abnormalities are benign and not causing significant symptoms. However, if symptoms are present or the underlying cause is concerning, treatment options may include medication management to control the heart rate or rhythm, such as beta-blockers or antiarrhythmic drugs. In certain instances, correction of the underlying causes, such as treating SA node dysfunction or managing AV block, may be necessary. In more severe cases, surgical interventions, such as implanting a pacemaker, may be considered.
| Causes of Junctional Rhythm | Symptoms of Junctional Rhythm | Treatment Options for Junctional Rhythm |
|---|---|---|
| SA node dysfunction | Palpitations | Medication management |
| AV block | Lightheadedness | Correction of underlying causes |
| Myocardial ischemia | Fatigue | Surgical interventions |
| Certain medications | Syncope |
Similarities between Idioventricular Rhythm and Junctional Rhythm
Idioventricular rhythm and junctional rhythm are both types of cardiac rhythms that arise when the normal pacemakers of the heart, such as the sinus node or AV node, are dysfunctional or blocked. Despite their differences in pacemaker location, these rhythms exhibit several similarities that can aid in their recognition and interpretation.
Firstly, both idioventricular rhythm and junctional rhythm are characterized by a regular rhythm on an ECG. This means that the R-R intervals between consecutive QRS complexes are consistent, providing a predictable pattern. This regularity can be helpful in distinguishing these rhythms from other irregular cardiac arrhythmias.
Secondly, both rhythms typically present with the absence of P waves on an ECG. In idioventricular rhythm, the P wave is often obscured or absent due to the abnormal pacemaker location within the ventricles. Similarly, junctional rhythm is characterized by inverted or absent P waves, indicating that the atrioventricular junction is responsible for initiating the electrical activity of the heart.
Lastly, idioventricular rhythm and junctional rhythm are generally considered benign rhythms. While they may be associated with underlying cardiac abnormalities or pathologies, they often do not require immediate treatment unless they cause symptoms or are accompanied by other significant cardiac issues. Therefore, it is crucial to evaluate the patient holistically and consider the clinical context when managing these rhythms.
| Similarities | Idioventricular Rhythm | Junctional Rhythm |
|---|---|---|
| Regular Rhythm | Yes | Yes |
| Absence of P waves | Yes | Yes |
| Benign Rhythm | Yes | Yes |
Differences between Idioventricular Rhythm and Junctional Rhythm
Idioventricular rhythm and junctional rhythm are distinct cardiac rhythms with different pacemaker locations and ECG findings. Understanding these differences is crucial for accurate EKG interpretation and differentiation between the two rhythms.
In idioventricular rhythm, the ventricles themselves act as the dominant pacemaker. This rhythm occurs when the normal pacemakers, such as the sinus node, are blocked or depressed. On the other hand, in junctional rhythm, the atrioventricular junction, specifically the AV node, becomes the pacemaker.
“The key difference between idioventricular rhythm and junctional rhythm lies in the location of the pacemaker.”
This difference in pacemaker location leads to different ECG findings. Idioventricular rhythm is characterized by the absence of P waves, while junctional rhythm may present with inverted or absent P waves. These distinctive ECG findings aid in distinguishing between the two rhythms and guiding appropriate management.
Table: Summary of Differences between Idioventricular Rhythm and Junctional Rhythm
| Characteristic | Idioventricular Rhythm | Junctional Rhythm |
|---|---|---|
| Location of Pacemaker | Ventricles | Atrioventricular Junction (AV Node) |
| ECG Findings | Absence of P Waves | Inverted or Absent P Waves |
Recognizing these differences is essential for accurate diagnosis and appropriate management of patients with idioventricular rhythm or junctional rhythm.
Evaluation and Diagnosis
Evaluation and diagnosis play a critical role in accurately identifying and distinguishing between idioventricular rhythm and junctional rhythm. This helps guide appropriate treatment and management strategies for patients with these cardiac arrhythmias.
ECG Evaluation
An electrocardiogram (ECG) is an essential tool in evaluating and diagnosing idioventricular rhythm and junctional rhythm. The ECG findings provide valuable information about the rate, rhythm, and conduction abnormalities within the heart. For idioventricular rhythm, the rate is typically less than 50 bpm, while junctional rhythm may have a rate between 40 to 60 bpm. These rates can help differentiate between the two rhythms.
Furthermore, the ECG interpretation focuses on specific features that are characteristic of each rhythm. In idioventricular rhythm, the absence of P waves and a prolonged QRS complex are key findings. Conversely, junctional rhythm is associated with inverted or absent P waves on the ECG. The recognition of these distinguishing features aids in the accurate diagnosis of each rhythm.
Clinical Correlation
In addition to the ECG evaluation, clinical correlation is necessary to interpret the significance of idioventricular rhythm and junctional rhythm. Patient history, symptoms, and physical examination findings provide valuable context in understanding the underlying causes and potential implications of these rhythms.
For instance, a patient with a history of myocardial infarction and an ECG showing idioventricular rhythm may indicate ischemic heart disease as the underlying cause. On the other hand, a patient with symptoms of lightheadedness and an ECG showing junctional rhythm may suggest dysfunction in the atrioventricular junction. The clinical correlation helps guide further diagnostic investigations and appropriate treatment options.
Treatment Guidelines
Treatment guidelines for idioventricular rhythm and junctional rhythm depend on several factors, including the underlying causes, severity of symptoms, and potential complications. In many cases, treatment may not be required if the rhythms are benign and asymptomatic.
However, if symptoms are present or the rhythms are associated with significant cardiac issues, intervention may be necessary. Treatment options may include medication management to control heart rate or correct rhythm abnormalities. In some cases, correction of underlying causes, such as electrolyte imbalances or myocardial ischemia, is essential. Surgical interventions, such as pacemaker implantation, may be considered for certain patients with severe rhythm abnormalities.
Overall, the evaluation and diagnosis of idioventricular rhythm and junctional rhythm involve a comprehensive approach that combines ECG evaluation, clinical correlation, and adherence to treatment guidelines. This allows healthcare professionals to provide appropriate care and management for patients with these cardiac arrhythmias.
| Idioventricular Rhythm | Junctional Rhythm | |
|---|---|---|
| Distinguishing Features | Absence of P waves Prolonged QRS complex |
Inverted or absent P waves |
| Rate | Less than 50 bpm | 40 to 60 bpm |
| ECG Findings | Absence of P waves, prolonged QRS complex | Inverted or absent P waves |
| Treatment | Treatment depends on underlying causes, severity of symptoms, and potential complications. | Treatment options include medication management, correction of underlying causes, and surgical interventions. |
Management and Treatment
Effective management and treatment of idioventricular rhythm and junctional rhythm focus on addressing the underlying causes and managing symptoms. By identifying and addressing the root causes, healthcare professionals can develop targeted treatment plans to improve the patient’s overall cardiac health and quality of life.
Underlying Causes
The first step in managing idioventricular rhythm and junctional rhythm is to identify and address any underlying causes. For idioventricular rhythm, potential causes can include medication toxicity, electrolyte imbalances, myocardial ischemia, and congenital heart diseases. In junctional rhythm, common causes may include SA node dysfunction, AV block, myocardial ischemia, or medication side effects. By treating or correcting the underlying causes, the abnormal rhythms can be better controlled or resolved.
Medication Management
In symptomatic patients or those with specific risk factors, medication management may be considered. Medications such as beta-blockers or calcium channel blockers are commonly used to control heart rate and rhythm abnormalities. The choice of medication depends on the individual patient and their specific needs. It is important to closely monitor patients on medications and adjust the dosage as necessary to achieve the desired therapeutic effect.
Correction of Electrolyte Imbalances and Surgical Interventions
In cases where idioventricular rhythm or junctional rhythm is caused by electrolyte imbalances, correcting these imbalances is crucial for effective management. Patients may require electrolyte replacement therapy or dietary modifications to ensure adequate levels of essential minerals and electrolytes. In some instances, surgical interventions may be necessary to address structural abnormalities or implant pacemakers to regulate the heart’s rhythm.
| Management Approach | Recommended Actions |
|---|---|
| Identify Underlying Causes | Thorough evaluation of medical history, diagnostic tests, and clinical correlation to determine the root causes of idioventricular rhythm or junctional rhythm. |
| Medication Management | Prescribe appropriate medications, such as beta-blockers or calcium channel blockers, to control heart rate and rhythm abnormalities. |
| Correction of Electrolyte Imbalances | Implement electrolyte replacement therapy or dietary modifications to restore proper electrolyte levels in patients with imbalances contributing to the abnormal rhythms. |
| Surgical Interventions | Consider surgical interventions, such as pacemaker implantation or corrective procedures, for structural abnormalities or refractory cases. |
In summary, the management and treatment of idioventricular rhythm and junctional rhythm involve addressing the underlying causes, medication management, correcting electrolyte imbalances, and, in some cases, surgical interventions. By implementing a comprehensive approach, healthcare professionals can help patients effectively manage their cardiac arrhythmias and improve their overall cardiac health.
Conclusion
In conclusion, understanding and distinguishing between idioventricular rhythm and junctional rhythm is crucial for the accurate interpretation and management of cardiac arrhythmias. Idioventricular rhythm is characterized by a slow regular ventricular rhythm, while junctional rhythm occurs when the atrioventricular junction acts as the pacemaker. Both rhythms have specific ECG findings and can be associated with various underlying causes.
Treatment strategies for these rhythm abnormalities focus on addressing reversible causes, managing symptoms, and correcting rhythm abnormalities. Medication management, correction of electrolyte imbalances, and surgical interventions may be employed depending on the individual case. It is important for healthcare professionals to consider the specific needs of each patient and develop personalized treatment plans.
In summary, by recognizing the differences and similarities between idioventricular rhythm and junctional rhythm, healthcare professionals can provide optimal EKG interpretation and implement effective treatment and management strategies for patients with heart rhythm disorders. With appropriate care and attention, individuals with these rhythm abnormalities can achieve better heart health and improved quality of life.
FAQ
What is idioventricular rhythm?
Idioventricular rhythm is a slow regular ventricular rhythm with a rate of less than 50 bpm. It occurs when the sinoatrial node is blocked or depressed, and the ventricles take over as the pacemaker.
What is junctional rhythm?
Junctional rhythm is an abnormal rhythm that occurs when the atrioventricular junction, specifically the AV node, acts as the pacemaker in the absence of normal sinus rhythm.
How are idioventricular rhythm and junctional rhythm diagnosed?
Idioventricular rhythm is diagnosed by an ECG that shows a slow regular ventricular rhythm with a prolonged QRS interval and absence of P waves. On the other hand, junctional rhythm is diagnosed by an ECG that shows inverted or absent P waves.
What are the causes of idioventricular rhythm?
Idioventricular rhythm can be caused by AV block, myocardial infarction, electrolyte imbalances, certain medications, congenital heart diseases, and a decrease in sympathetic tone in athletes.
What are the common causes of junctional rhythm?
Common causes of junctional rhythm include SA node dysfunction, AV block, myocardial ischemia, and certain medications.
What are the treatment options for idioventricular rhythm and junctional rhythm?
Treatment options for both rhythms depend on the severity of symptoms and may include medication management, correction of underlying causes, and in some cases, surgical interventions or pacemaker implantation.
Are idioventricular rhythm and junctional rhythm considered benign?
Yes, both rhythms are generally considered benign and do not always require immediate treatment unless they cause symptoms or are associated with other significant cardiac issues.