When it comes to pain relief during labor or surgical procedures involving the spine, two commonly used techniques are spinal anesthesia and epidural anesthesia. While these methods may seem similar, there are key differences that set them apart.
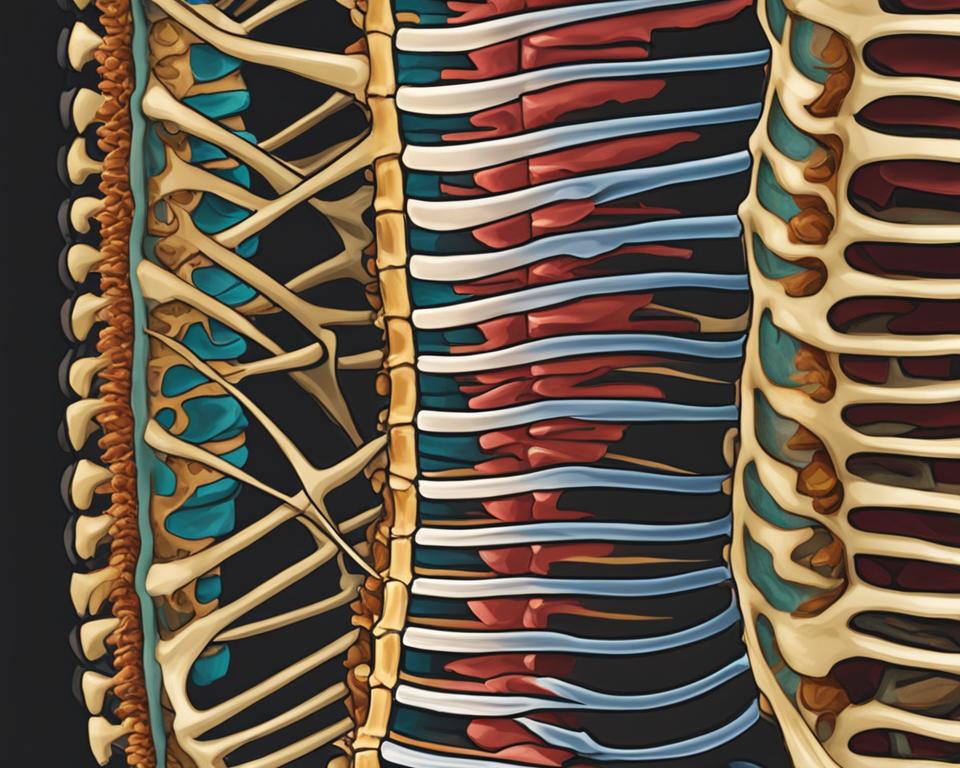
Spinal anesthesia involves the injection of numbing medicine directly into the fluid sac surrounding the spinal cord, while epidural anesthesia involves the injection into the space outside the sac. Both techniques numb a large region of the body, but the spinal injection has a more immediate effect.
Spinals are commonly used for Cesarean deliveries, while epidurals are preferred for pain relief during labor. The effect of a spinal is usually shorter, lasting about 1-2 hours, compared to the continuous infusion possible with an epidural catheter.
Key Takeaways:
- Spinal anesthesia involves injecting medicine into the fluid sac surrounding the spinal cord, while epidural anesthesia involves injecting medicine into the space outside the sac.
- Spinals have a more immediate effect and are commonly used for Cesarean deliveries, while epidurals provide continuous pain relief during labor.
- Spinal anesthesia lasts for about 1-2 hours, while epidural anesthesia can be continuously infused.
- Both techniques have their uses, and the choice depends on the specific procedure and individual preferences.
- It is important to discuss any allergies or health conditions with the anesthesiologist prior to the procedure.
How Are Spinal And Epidural Anesthesia Given?
Spinal anesthesia and epidural anesthesia are both administered through shots in or around the spine. For an epidural, medicine is injected just outside the sac of fluid around the spinal cord, while a spinal involves injecting medicine into the fluid that surrounds the spinal cord. The medications used are usually a combination of local anesthetics and/or narcotics. Epidurals often involve the placement of a catheter for continuous infusion, while spinals are typically a one-time injection.
When performing a spinal anesthesia procedure, the healthcare provider will have the patient sit or lie on their side with their back arched. After cleaning and numbing the injection site, a needle is carefully inserted into the spinal fluid. The medicine is then injected, which numbs the nerves responsible for pain sensation in the lower body.
In contrast, an epidural anesthesia procedure involves a similar initial setup, with the patient positioned and the injection site cleaned and numbed. However, instead of injecting directly into the spinal fluid, the healthcare provider advances a needle through the back muscles and ligaments until it reaches the epidural space just outside the sac of fluid surrounding the spinal cord. The medicine is then injected into this space, where it spreads and provides pain relief to a larger area of the body.
| Procedure | Spinal Anesthesia | Epidural Anesthesia |
|---|---|---|
| Injection Site | Into the spinal fluid | Outside the sac of fluid surrounding the spinal cord |
| Medication | One-time injection of a combination of local anesthetics and/or narcotics | Possible continuous infusion of medication through a catheter |
“Spinal anesthesia involves injecting the medication directly into the spinal fluid, resulting in a more immediate effect. Epidural anesthesia, on the other hand, is administered outside the sac of fluid surrounding the spinal cord, offering the possibility of continuous infusion for prolonged pain relief.”
It is important to note that the specific technique and medication used may vary depending on the healthcare provider’s preference and the patient’s needs. The decision between spinal and epidural anesthesia should be made in consultation with an anesthesiologist, who will consider various factors such as the nature of the procedure, the patient’s medical history, and their preferences in order to provide the most appropriate and effective pain relief.
Differences in Onset and Duration
When it comes to spinal and epidural anesthesia, there are notable differences in both the onset and duration of pain relief. Understanding these differences can help patients and healthcare professionals make informed decisions regarding the appropriate anesthesia technique for specific procedures.
Onset
The onset of spinal anesthesia is relatively fast, typically within minutes after the injection. This means that patients can experience immediate pain relief, making it particularly effective for procedures requiring quick and efficient anesthesia. On the other hand, epidural anesthesia takes slightly longer to establish the desired effect, usually within 10-20 minutes. While the onset may be slower compared to spinal anesthesia, it still provides effective pain relief within a reasonable timeframe.
Duration
Although spinal anesthesia offers a rapid onset, the duration of pain relief is relatively short. Typically, spinal anesthesia lasts about 1-2 hours, making it suitable for procedures that require shorter periods of pain management. In contrast, epidural anesthesia can provide pain relief for a longer duration. The continuous infusion made possible with an epidural catheter allows for a steady flow of medication, providing prolonged pain relief for patients.
When deciding between spinal and epidural anesthesia, it is crucial to consider the specific requirements of the procedure and individual patient needs. While spinal anesthesia offers immediate pain relief, it may be more suitable for shorter procedures. On the other hand, epidural anesthesia provides a longer-lasting pain management solution, making it ideal for procedures that require continuous pain relief over an extended period of time.
Ultimately, the choice between spinal and epidural anesthesia should be made in consultation with an anesthesiologist, who can provide personalized recommendations based on the patient’s medical history, procedure requirements, and individual preferences.
Uses and Applications of Spinal and Epidural Anesthesia
Spinal and epidural anesthesia are widely used in various medical procedures, including labor and delivery and surgical interventions. Each technique has its own specific applications and benefits, tailored to meet the needs of patients. Understanding the uses and applications of spinal and epidural anesthesia can help individuals make informed decisions regarding their anesthesia options.
Uses in Labor and Delivery
Both spinal and epidural anesthesia play crucial roles in providing pain relief during labor and delivery. Epidurals are commonly used to manage labor pain, as they allow for continuous infusion of medication through a catheter. This provides ongoing pain relief while maintaining the ability to move and push during childbirth. Spinal anesthesia, on the other hand, is often preferred for Cesarean deliveries as it provides rapid and effective anesthesia to the lower body, allowing for surgical procedures to be performed without discomfort or pain.
Applications in Surgical Procedures
Spinal and epidural anesthesia are also frequently used in various surgical procedures. Spinal anesthesia is particularly beneficial for surgeries involving the lower body, genital, and urinary tract. It can provide precise anesthesia to these regions, ensuring patient comfort and pain control during the procedure. Epidural anesthesia, on the other hand, is commonly used for surgical interventions in the pelvis and legs. Its ability to deliver continuous pain relief makes it an ideal choice for longer surgeries where prolonged anesthesia is needed.
| Spinal Anesthesia | Epidural Anesthesia | |
|---|---|---|
| Labor and Delivery | Preferred for Cesarean deliveries | Commonly used for pain relief during labor |
| Surgical Procedures | Lower body, genital, and urinary tract surgeries | Pelvic and leg surgeries |
When considering the use of spinal or epidural anesthesia for a specific surgical procedure, it is important to consult with an anesthesiologist. They will assess the individual’s medical history, the nature of the procedure, and other factors to determine the most appropriate anesthesia option for optimal patient outcomes.
Safety and Possible Complications
When it comes to spinal and epidural anesthesia, it is essential to be aware of the potential complications that can arise. While these procedures are generally safe, there are several risks that patients should understand.
One possible complication is an allergic reaction to the anesthesia. It is important to inform the anesthesiologist of any known allergies prior to the procedure to ensure appropriate measures are taken.
Bleeding around the spinal column is another potential risk. Although rare, it can occur and may require medical attention. Monitoring for any signs of excessive bleeding is crucial during and after the administration of spinal or epidural anesthesia.
Another complication that can arise is a drop in blood pressure. The medications used for anesthesia can sometimes cause a temporary decrease in blood pressure. However, healthcare professionals closely monitor blood pressure levels during the procedure to address any fluctuations promptly.
Infection in the spine is another risk associated with spinal and epidural anesthesia. Although rare, it is imperative to follow sterile techniques during these procedures to minimize the chances of infection.
Nerve damage is a potential complication that can occur, resulting in sensory or motor deficits. Healthcare providers take great care to minimize the risk of nerve damage by utilizing proper technique and ensuring accurate needle placement.
Finally, in rare cases, patients may experience a post-procedure headache known as a spinal headache. This headache can be severe and may require additional medical interventions for relief.
Table: Possible Complications of Spinal and Epidural Anesthesia
| Complication | Description |
|---|---|
| Allergic Reaction | An adverse response to the anesthesia drugs, requiring immediate medical attention. |
| Bleeding | Excessive bleeding around the spinal column, which can necessitate further treatment. |
| Drop in Blood Pressure | A temporary decrease in blood pressure, often monitored and managed during the procedure. |
| Infection | An infection in the spine, which is a rare but serious complication. |
| Nerve Damage | Possible damage to nerves resulting in sensory or motor deficits. |
| Spinal Headache | A severe headache that can occur after the procedure, requiring additional treatment. |
Conclusion
In summary, when it comes to spinal and epidural anesthesia, there are distinct differences to consider. Spinal anesthesia offers a quicker onset of pain relief, making it ideal for situations that require immediate numbing. However, the duration of pain relief is shorter, typically lasting around 1 to 2 hours.
Epidural anesthesia, on the other hand, may take slightly longer to take effect, but it allows for continuous infusion of medication, resulting in prolonged pain relief. This makes it a popular choice for labor and delivery, as well as for surgical procedures involving the pelvis and legs.
When deciding between spinal and epidural anesthesia, it is important to weigh the benefits and considerations of each approach. Spinal anesthesia offers fast relief, but it may not be suitable for procedures requiring longer-lasting numbing. Epidural anesthesia provides continuous pain relief, but it may take slightly longer to establish the desired effect.
Ultimately, the choice of anesthesia technique depends on the specific procedure and individual preferences. It is essential to consult with an anesthesiologist who can provide expert guidance and help determine the best option for each patient.
FAQ
How is spinal anesthesia given?
Spinal anesthesia involves the injection of numbing medicine directly into the fluid sac surrounding the spinal cord.
How is epidural anesthesia given?
Epidural anesthesia involves the injection of numbing medicine just outside the sac of fluid around the spinal cord.
What is the difference in the onset and duration of spinal and epidural anesthesia?
Spinal anesthesia has a faster onset, providing pain relief within minutes, but lasts for a shorter duration of about 1-2 hours. Epidural anesthesia takes slightly longer to take effect, usually within 10-20 minutes, but can provide continuous pain relief for a longer duration.
What are the uses of spinal and epidural anesthesia?
Spinal anesthesia is commonly used for surgical procedures involving the lower body, genital, and urinary tract. It is often the anesthesia of choice for Cesarean deliveries. Epidural anesthesia is frequently used for pain relief during labor and delivery and can also be used for surgical procedures in the pelvis and legs.
What are the possible complications of spinal and epidural anesthesia?
Possible complications include allergic reactions, bleeding around the spinal column, difficulty urinating, drop in blood pressure, infection in the spine, nerve damage, and in rare cases, seizures or severe headaches.

