Welcome to our informative article on the difference between ulcerative colitis (UC) and Crohn’s disease (CD), the two main forms of inflammatory bowel diseases. If you’ve been diagnosed with either condition or suspect you may have symptoms related to them, it’s essential to understand their distinctions for accurate diagnosis, appropriate treatment, and disease management.
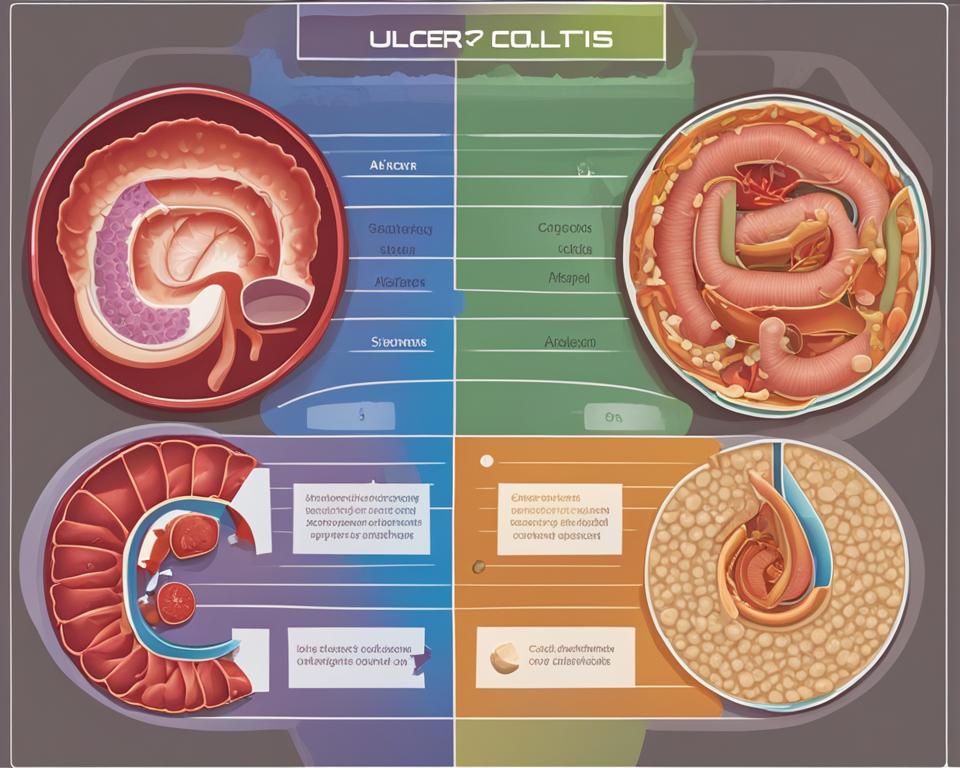
Ulcerative colitis and Crohn’s disease share similarities in terms of age of onset, gender distribution, and symptoms, but there are key differences. Ulcerative colitis is limited to the colon, while Crohn’s disease can affect any part of the digestive tract. The extent and location of inflammation also vary, with ulcerative colitis impacting only the innermost lining of the colon and Crohn’s disease potentially involving all layers of the bowel walls. Additionally, approximately 10% of inflammatory bowel disease cases exhibit features of both Crohn’s disease and ulcerative colitis, known as indeterminate colitis.
Key Takeaways:
- Ulcerative colitis is limited to the colon, while Crohn’s disease can affect any part of the digestive tract.
- The extent and location of inflammation differ between the two diseases.
- Approximately 10% of inflammatory bowel disease cases exhibit features of both Crohn’s disease and ulcerative colitis.
Symptoms of Ulcerative Colitis and Crohn’s Disease
Individuals with ulcerative colitis and Crohn’s disease may experience similar symptoms, but there are distinct differences between the two conditions. Here are the common symptoms associated with each:
Symptoms of Ulcerative Colitis:
- Abdominal pain
- Diarrhea, often with blood
- Rectal bleeding
- Fatigue
- Weight loss
- Rectal urgency and tenesmus (feeling the need to pass stool even when the rectum is empty)
Symptoms of Crohn’s Disease:
- Abdominal pain and cramping
- Diarrhea
- Frequent bowel movements
- Fatigue
- Weight loss
- Inflammation in various parts of the digestive tract
The specific symptoms and their severity can vary depending on the location and extent of inflammation in each individual. It is important to note that some individuals may experience symptoms outside of the gastrointestinal tract, such as joint pain, skin rashes, and eye inflammation, which can also occur in Crohn’s disease.
Consulting with a healthcare professional is essential for accurate diagnosis and appropriate management of symptoms.
| Symptoms of Ulcerative Colitis | Symptoms of Crohn’s Disease | |
|---|---|---|
| Abdominal Pain | ✔ | ✔ |
| Diarrhea | ✔ | ✔ |
| Rectal Bleeding | ✔ | |
| Fatigue | ✔ | ✔ |
| Weight Loss | ✔ | ✔ |
| Rectal Urgency and Tenesmus | ✔ | |
| Inflammation in Various Digestive Tract Areas | ✔ |
Causes of Ulcerative Colitis and Crohn’s Disease
The exact causes of ulcerative colitis and Crohn’s disease are still unknown. However, research suggests that these conditions result from a combination of genetic, environmental, and immune system factors.
Genetics play a significant role in the development of ulcerative colitis and Crohn’s disease. Having a family history of inflammatory bowel disease increases the risk of developing these conditions. Certain gene mutations may make individuals more susceptible to chronic inflammation in the digestive tract.
Environmental factors also contribute to the onset of ulcerative colitis and Crohn’s disease. Infections, such as bacterial or viral gastroenteritis, can trigger an abnormal immune response in susceptible individuals, leading to inflammation in the digestive tract. Additionally, dietary factors may play a role, although specific triggers vary among individuals.
A study published in the Journal of Gastroenterology and Hepatology found that a diet high in processed foods and low in fiber may increase the risk of developing Crohn’s disease. On the other hand, diets rich in fruits, vegetables, and omega-3 fatty acids appear to have a protective effect against both ulcerative colitis and Crohn’s disease.
The immune system also plays a crucial role in the development of ulcerative colitis and Crohn’s disease. In individuals with these conditions, the immune system mistakenly identifies harmless substances, such as food particles or intestinal bacteria, as threats. This triggers an immune response that leads to chronic inflammation in the digestive tract, causing the characteristic symptoms of ulcerative colitis and Crohn’s disease.
It’s important to note that while these factors are believed to contribute to the development of ulcerative colitis and Crohn’s disease, they do not guarantee the onset of the conditions. Each individual may have a unique combination of genetic susceptibility, environmental triggers, and immune system responses that contribute to their specific disease presentation.
Treatment Options for Ulcerative Colitis
When it comes to managing ulcerative colitis, there are several treatment options available. The goal of treatment is to reduce inflammation, alleviate symptoms, and promote healing of the affected tissues. The specific approach to treatment may vary depending on the severity and location of inflammation, as well as individual patient factors.
Medications are commonly used to manage ulcerative colitis. These may include:
- Biologics: These are antibodies that help fight inflammation. They target specific molecules in the immune system to reduce inflammation and promote healing.
- Immunomodulators: These medications help regulate the immune system and prevent it from attacking the digestive tract. They can be effective in keeping the disease in remission.
- Aminosalicylates: These drugs work by reducing inflammation in the colon. They are often used as a first-line treatment for mild to moderate ulcerative colitis.
- Janus kinase inhibitors: These medications target specific enzymes involved in the inflammatory process. They can help reduce inflammation and alleviate symptoms in some individuals.
In some cases, surgery may be necessary for ulcerative colitis, particularly for severe disease or complications that do not respond to medication. Surgical options may include a colectomy, which involves removing the colon and creating an internal pouch that functions similarly to the colon. Advances in medical care have significantly reduced the number of colectomies required for ulcerative colitis, but it may still be necessary in certain cases.
| Treatment Option | Description |
|---|---|
| Biologics | Antibodies that fight inflammation |
| Immunomodulators | Regulate the immune system |
| Aminosalicylates | Reduce inflammation in the colon |
| Janus kinase inhibitors | Target enzymes involved in inflammation |
It’s important for individuals with ulcerative colitis to work closely with their healthcare team to determine the most appropriate treatment plan for their specific situation. Regular monitoring and adjustments to the treatment approach may be necessary to effectively manage the disease.
Surgery for Ulcerative Colitis and Crohn’s Disease
For some individuals with ulcerative colitis and Crohn’s disease, surgery may be necessary to manage the conditions effectively. Surgical interventions play a vital role in eliminating or reducing the symptoms and complications associated with these inflammatory bowel diseases.
In ulcerative colitis cases, a procedure called colectomy may be performed. This surgery involves removing the colon and creating an internal pouch that functions similarly to the colon. Colectomy is highly effective in eliminating the disease and providing long-term relief. However, advancements in medical care have significantly reduced the number of colectomies required for ulcerative colitis, as other treatment options have become more successful.
For individuals with Crohn’s disease, surgery aims to remove the inflamed sections of the digestive tract while preserving as much healthy tissue as possible. This surgical intervention helps alleviate symptoms and prevent complications. In some cases, surgical repair may also be necessary for fistulas, which are abnormal tunnels between different sections of the bowel.
| Surgery for Ulcerative Colitis | Surgery for Crohn’s Disease |
|---|---|
| Colectomy: Removal of the colon with the creation of an internal pouch | Resection: Removal of inflamed sections of the digestive tract |
| Preservation of as much healthy tissue as possible | |
| Surgical repair of fistulas if present |
The decision for surgery depends on various factors, including the individual’s response to medication, the severity of the disease, and the presence of complications. It is essential for healthcare professionals to evaluate each case thoroughly and determine the most appropriate course of action to ensure optimal outcomes for patients.
Impact on Diet
Diet plays a significant role in managing symptoms and preventing flare-ups for both ulcerative colitis and Crohn’s disease. While there are no universal dietary guidelines, individuals with these conditions may find that certain foods trigger their symptoms. High-fiber vegetables, uncooked produce, unpeeled fruits, dairy products, and fatty or greasy foods are often challenging to digest for those with inflammatory bowel disease. Working with a dietitian can help individuals identify their specific trigger foods and develop a plan that supports their digestive health.
“I’ve noticed that when I eat greasy foods, my symptoms worsen. So I try to avoid fried foods and opt for lighter options like grilled chicken or fish,” says Sarah, a Crohn’s disease patient.
It is important to note that individual responses to certain foods may vary, and what triggers symptoms in one person may not affect another. Keeping a food diary can be helpful in identifying patterns and making necessary adjustments to one’s diet. Alongside diet modifications, healthcare professionals may also recommend dietary supplements to ensure proper nutrient intake and support overall gastrointestinal health.
While diet can play a role in symptom management, it is essential to consult with a healthcare professional or registered dietitian to create a personalized diet plan that meets individual needs. These professionals can provide guidance on nutrition, monitor nutrient deficiencies, and make recommendations based on an individual’s specific condition and medical history.
| Ulcerative Colitis | Crohn’s Disease | |
|---|---|---|
| Trigger Foods | High-fiber vegetables, uncooked produce, unpeeled fruits, dairy products, fatty or greasy foods | High-fiber foods, spicy foods, alcohol, caffeine, fried foods |
| Recommended Foods | Low-fiber foods, cooked vegetables, peeled fruits, lean proteins, well-cooked grains | Low-fiber foods, lean proteins, cooked fruits and vegetables, soft foods |
| Supplements | Iron, vitamin B12, calcium, vitamin D | Vitamin B12, vitamin D, calcium, omega-3 fatty acids |
Overall, maintaining a well-balanced diet that focuses on easy-to-digest foods and avoids trigger foods can help individuals with ulcerative colitis and Crohn’s disease manage their symptoms and improve their quality of life.
Indeterminate Colitis
Indeterminate colitis is a term used to describe approximately 10% of cases of inflammatory bowel disease that exhibit features of both Crohn’s disease and ulcerative colitis. It presents a challenge in diagnosis and treatment as the characteristics of the disease do not clearly align with either condition. Patients with indeterminate colitis often require close monitoring and a multidisciplinary approach to develop personalized treatment strategies.
The identification of indeterminate colitis often occurs when the characteristics of the disease do not fit the typical patterns observed in either Crohn’s disease or ulcerative colitis. In these cases, patients may exhibit symptoms and findings that are characteristic of both diseases, making an accurate diagnosis difficult. Additional diagnostic tests, such as imaging studies and endoscopy, may be necessary to gather more information and rule out other potential causes of the symptoms.
Given the unique nature of indeterminate colitis, treatment approaches are personalized based on the individual’s symptoms, disease severity, and response to therapy. The goal is to reduce inflammation, alleviate symptoms, and promote healing of the affected tissues. Treatment options may include medications commonly used for Crohn’s disease or ulcerative colitis, such as aminosalicylates, immunomodulators, and biologics. In some cases, surgery may be necessary if the disease is severe or complications arise that do not respond to medication.
In conclusion, indeterminate colitis is a subset of inflammatory bowel disease that presents a challenge in diagnosis and treatment. It requires a comprehensive evaluation, close monitoring, and personalized treatment strategies tailored to the individual patient. Ongoing research and advancements in understanding the underlying mechanisms of the disease may lead to improved diagnostic techniques and targeted therapies for individuals with indeterminate colitis.
Conclusion
In conclusion, ulcerative colitis and Crohn’s disease are both forms of inflammatory bowel diseases with distinct differences. Ulcerative colitis is limited to the colon, while Crohn’s disease can affect any part of the digestive tract. The extent and location of inflammation also vary, with ulcerative colitis affecting only the innermost lining of the colon and Crohn’s disease potentially impacting all layers of the bowel walls.
Understanding these differences is crucial for accurate diagnosis, appropriate treatment, and disease management. If you suspect you may have any symptoms or concerns related to ulcerative colitis or Crohn’s disease, it is important to consult with a healthcare professional for proper evaluation and guidance. They can provide the necessary expertise and advice to help manage your condition effectively.
With the right treatment and support, individuals living with ulcerative colitis or Crohn’s disease can lead healthy and fulfilling lives. Remember, you are not alone in this journey, and healthcare professionals are there to support you every step of the way.
FAQ
What is the difference between ulcerative colitis and Crohn’s disease?
Ulcerative colitis is limited to the colon, while Crohn’s disease can affect any part of the digestive tract. Additionally, the extent and location of inflammation differ between the two diseases.
What are the symptoms of ulcerative colitis and Crohn’s disease?
Symptoms can include abdominal pain, diarrhea, rectal bleeding, fatigue, and weight loss. The specific symptoms and their severity may vary depending on the individual and the location of inflammation.
What causes ulcerative colitis and Crohn’s disease?
The exact causes are unknown, but a combination of genetic, environmental, and immune system factors are believed to be involved. Family history and environmental triggers may contribute to the development of these diseases.
What are the treatment options for ulcerative colitis and Crohn’s disease?
Treatment aims to reduce inflammation, alleviate symptoms, and promote healing. Medications such as biologics, immunomodulators, aminosalicylates, and Janus kinase inhibitors are commonly used. In some cases, surgery may be necessary.
Is surgery required for ulcerative colitis and Crohn’s disease?
In some cases, surgery may be necessary, particularly for severe disease or complications that do not respond to medication. Colectomy, which involves removing the colon, may be performed for ulcerative colitis, while in Crohn’s disease, surgery aims to remove the inflamed sections of the digestive tract.
How does diet impact ulcerative colitis and Crohn’s disease?
Diet plays a significant role in managing symptoms and preventing flare-ups. While there are no universal guidelines, individuals may find that certain foods trigger their symptoms. Working with a dietitian can help identify specific trigger foods and develop a personalized plan.
What is indeterminate colitis?
Indeterminate colitis refers to approximately 10% of inflammatory bowel disease cases that exhibit features of both Crohn’s disease and ulcerative colitis. These cases present challenges in diagnosis and treatment.

