Allergy testing is a crucial step in identifying the specific allergens responsible for allergic reactions. It helps determine the substances that trigger symptoms and enables healthcare professionals to develop an effective treatment plan.
Allergy testing involves exposing the skin to suspected allergy-causing substances, known as allergens, and observing for signs of an allergic reaction. By doing so, it confirms whether a particular substance is causing the symptoms and helps pinpoint the allergens that need to be addressed.
Commonly used for diagnosing allergic conditions such as hay fever, allergic asthma, dermatitis, food allergies, penicillin allergy, and bee venom allergy, skin tests are the primary method utilized in allergy testing. However, they may not be suitable for individuals with certain medical conditions or medications that interfere with the test results.
Key Takeaways:
- Allergy testing involves exposing the skin to allergens to observe for signs of an allergic reaction.
- Skin tests are commonly used for diagnosing allergic conditions.
- Other diagnostic methods include blood tests.
- The choice of testing method depends on factors such as symptoms, medical history, and specific allergens of interest.
- Accurate interpretation of allergy test results is essential for diagnosis and developing a personalized treatment plan.
Allergy Testing Methods
Allergy testing can be done using different methods, including skin tests and blood tests. Each testing method has its own advantages and limitations and is chosen based on the patient’s symptoms, medical history, and specific allergens of interest.
Skin Tests
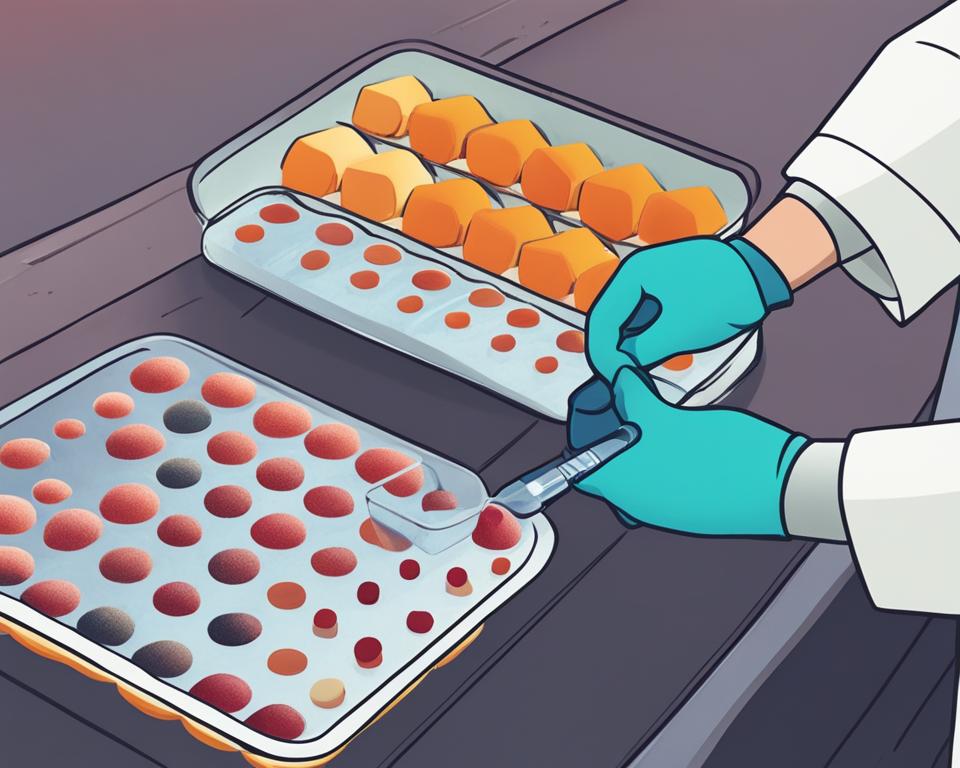
Skin tests, such as prick or scratch tests, involve pricking or scratching the skin with allergen extracts to observe for allergic reactions. Intradermal tests may be used to check for allergies to insect venom or penicillin. Patch tests are used to detect delayed allergic reactions.
Blood Tests
Blood tests, such as RAST or ELISA, measure IgE antibodies to allergens in the blood. Blood tests are often used when skin tests cannot be performed, such as in patients with certain skin conditions or recent severe allergic reactions.
The choice of test depends on the patient’s symptoms, medical history, and specific allergens of interest. Skin tests are generally preferred due to their accuracy and cost-effectiveness. However, in certain situations, blood tests may be necessary, especially in individuals unable to undergo skin tests.
| Testing Method | Advantages | Limitations |
|---|---|---|
| Skin Tests | – Can be done in a clinic setting – Immediate results – Cost-effective |
– May not be recommended for individuals with certain skin conditions or medications that interfere with test results |
| Blood Tests | – Can be performed when skin tests cannot be done – Useful for patients with certain skin conditions or recent severe allergic reactions |
– Results take longer to obtain compared to skin tests – May be more expensive |
Skin Testing Procedure
Allergy testing through skin tests is a common diagnostic procedure used to identify specific allergens causing allergic reactions. This method involves applying allergen extracts to the skin and observing for signs of an allergic reaction. The accuracy of skin testing is essential in providing accurate diagnosis and developing appropriate treatment plans for patients.
The skin testing procedure is typically performed in a doctor’s office by a trained professional. The allergen extracts are applied to the skin, usually on the forearm or upper back, and the skin is then pricked or scratched to allow the allergen to penetrate the surface. The response of the skin is observed, looking for raised, red, itchy bumps that indicate an allergic reaction. To ensure the accuracy of the test, control substances such as histamine and glycerin or saline are also used.
While skin testing is generally safe and provides fast results, it is important to note that false-positive and false-negative results can occur. The accuracy of the test may vary depending on the skill of the tester and the specific allergen being tested. It is crucial to have an experienced professional conducting the test to minimize the risk of inaccurate results. Skin testing remains a valuable tool in diagnosing allergies and plays a vital role in guiding the development of personalized treatment plans for patients.
| Allergy Testing Method | Advantages | Limitations |
|---|---|---|
| Skin Tests (Prick or Scratch Tests) | Fast results; cost-effective; can test for a wide range of allergens; immediate reactions can be observed | May not be recommended for individuals with severe allergic reactions, certain medications, or specific skin conditions; false-positive and false-negative results can occur |
| Intradermal Tests | Can detect allergies to insect venom or penicillin | Requires an additional step of injecting the allergen under the skin; may cause more discomfort and risk of adverse reactions |
| Patch Tests | Detects delayed allergic reactions | Requires multiple visits and longer observation periods; false-positive and false-negative results can occur |
| Blood Tests (RAST or ELISA) | No risk of allergic reactions; can be performed even when skin tests cannot | Results take longer to obtain; may be more expensive; may have limitations in detecting certain allergens |
Allergy Testing: Understanding the Blood Testing Procedure
While skin testing is the most common method for diagnosing allergies, blood testing is an alternative option that can provide valuable insights into allergen-specific IgE antibodies in the bloodstream. Blood testing for allergies, such as the RAST or ELISA test, is particularly useful for individuals who cannot undergo skin tests due to certain skin conditions or recent severe allergic reactions.
When performing a blood test, a healthcare professional will draw a blood sample from the patient’s arm. The sample is then sent to a laboratory where it is analyzed for the presence of IgE antibodies to specific allergens. The results of the blood test typically take longer to obtain compared to skin tests, as the analysis requires more time and specialized equipment.
The blood test results indicate whether there are IgE antibodies present in the blood that react to specific allergens. However, it is important to note that a positive blood test does not necessarily confirm an allergic reaction. Further interpretation and consideration of the patient’s medical history are essential to make an accurate diagnosis. By combining the results of the blood test with other clinical information, healthcare professionals can develop a comprehensive understanding of the patient’s allergies and create an effective treatment plan.
Allergy Testing for Adults: Making Informed Decisions
When it comes to allergy testing for adults, the choice between skin tests and blood tests depends on various factors. Skin tests are generally preferred due to their accuracy and cost-effectiveness. However, certain circumstances may warrant the use of blood tests. Adults who have skin conditions that make it difficult to perform skin tests or those who have experienced severe allergic reactions may be better suited for blood testing.
It’s important for adults to communicate openly with their healthcare providers about their medical history and any concerns they may have. By understanding the pros and cons of different allergy testing methods, adults can work together with their healthcare team to make informed decisions and ensure accurate allergy diagnosis.
Choosing the Right Test
Selecting the right allergy test is crucial for accurately diagnosing allergies and developing an effective treatment plan. Allergists consider various factors when choosing the most appropriate test for each individual. This includes the patient’s symptoms, medical history, age, environmental and occupational exposures, and the specific allergens of interest. By carefully evaluating these factors, allergists can determine whether skin tests or blood tests are more suitable for diagnosing the allergies.
In general, skin tests are preferred due to their accuracy and cost-effectiveness. They involve applying allergen extracts to the skin and observing the reaction. However, in some situations, such as individuals with certain skin conditions or recent severe allergic reactions, blood tests may be necessary. Blood tests measure the presence of immunoglobulin E (IgE) antibodies to specific allergens in the blood, providing valuable information for diagnosing allergies.
Allergy tests for children are safe and can be performed at any age, including infants. The choice of test for children is based on factors such as their symptoms, medical history, and exposure to potential allergens. Pediatric allergists are specially trained to perform allergy tests on children, ensuring accurate results and appropriate treatment plans.
Comparison of Skin Tests and Blood Tests
To better understand the differences between skin tests and blood tests, let’s compare them in a table:
| Aspect | Skin Tests | Blood Tests |
|---|---|---|
| Procedure | Application of allergen extracts to the skin | Blood sample collection |
| Accuracy | High | High |
| Results | Immediate | Delayed |
| Preparation | Avoid medications that may interfere with the test | No preparation required |
| Potential Risks | Slight redness or itching at the test site | No risks associated with the test itself |
It’s important to note that both skin tests and blood tests are valuable diagnostic tools. The choice between the two depends on individual circumstances and the expertise of the allergist. By selecting the most appropriate test, allergists can accurately diagnose allergies and create personalized treatment plans to effectively manage the symptoms.
Allergy Test Results Interpretation
Allergy test results are crucial for accurately diagnosing allergies and developing effective treatment plans. When interpreting test results, it is important to consider the patient’s medical history and symptoms. A positive test indicates the presence of IgE antibodies to a specific allergen, suggesting an allergy. However, false-positive and false-negative results can occur, so clinical judgment is necessary for accurate diagnosis.
The size of the allergic reaction on skin tests can indicate the degree of sensitivity to a particular allergen. A larger reaction may suggest a higher level of sensitivity. However, it is important to note that negative results do not necessarily mean the absence of an allergy. Allergic reactions can vary, and a patient may not react to an allergen on one occasion but react on another.
Expertise and clinical judgment, combined with the patient’s medical history and symptoms, are crucial for accurate allergy diagnosis. The allergist will consider all these factors when interpreting test results and making a final diagnosis. This comprehensive approach ensures that patients receive the most appropriate treatment and management plans tailored to their specific needs.
Role of Medical History in Allergy Diagnosis
In diagnosing allergies, medical history plays a vital role. It provides important information about the patient’s overall health, experiences with possible allergens, and symptoms at different times of the year. The allergist considers the medical history alongside the results of allergy tests to make a final diagnosis. Medical history helps establish a connection between allergy test results and allergic disease. It guides the allergist in developing appropriate therapies, management plans, and treatments tailored to each patient’s specific needs.
A thorough medical history allows the allergist to gather information about the patient’s symptoms, their duration and severity, triggers, and any previous treatments or interventions. This information helps build a comprehensive picture of the patient’s allergic history, which is crucial for accurate diagnosis and effective management. Allergists will also explore any family history of allergies, as there may be a genetic predisposition to certain allergic conditions.
Why is Medical History Important in Allergy Diagnosis?
Medical history helps allergists understand the context of an individual’s symptoms and provides valuable insights into potential allergens. For example, knowledge of a patient’s occupation may reveal exposure to specific allergens, such as chemicals or dust. Understanding the timing and seasonal variations of symptoms can indicate triggers related to outdoor allergies, such as pollen. The duration and severity of symptoms can also indicate the severity of the underlying allergic condition.
By combining medical history with the results of allergy tests, allergists can accurately diagnose the specific allergens responsible for a patient’s symptoms. This allows for targeted treatment plans that address the root cause of the allergies. It also helps rule out other potential causes of symptoms, ensuring that patients receive the appropriate care and management strategies.
Overall, the role of medical history in allergy diagnosis is crucial for accurate and effective treatment. By considering the patient’s medical history alongside allergy test results, allergists can develop personalized treatment plans that address the unique needs of each individual. This comprehensive approach leads to better management of allergies, improved quality of life, and reduced symptoms for patients.
Allergy Testing: Risks and Accuracy
Allergy testing, while an important diagnostic tool, does come with certain risks and challenges that need to be considered. It is crucial to be aware of these factors to ensure accurate and safe testing for individuals.
Risks: The most common side effect of skin testing is slightly swollen, red, itchy bumps at the test site. However, in rare cases, a severe allergic reaction can occur, requiring immediate access to emergency equipment and medications. It is essential to have trained professionals and emergency measures in place during allergy testing procedures.
Challenges: Several factors can affect the accuracy of allergy test results. Medications like antihistamines and specific antidepressants can interfere with the tests and may need to be temporarily discontinued to obtain more accurate results. Skin conditions and the skill of the tester can also impact the interpretation of test results. These challenges highlight the importance of choosing a qualified healthcare professional for allergy testing.
Allergy Testing Accuracy
While allergy testing is a valuable diagnostic tool, it’s important to note that there can be false-positive and false-negative results. Allergy test results should be interpreted in conjunction with the patient’s medical history and symptoms. The size of the allergic reaction observed during skin testing may indicate the degree of sensitivity. Conversely, negative results may indicate the absence of an allergy, but reactions can vary on different occasions.
It is crucial for healthcare professionals to have expertise, clinical judgment, and a comprehensive understanding of the patient’s medical history to accurately diagnose allergies based on test results.
Despite these challenges, accurate allergy testing plays a vital role in developing personalized treatment plans. Allergy test results guide healthcare professionals in recommending appropriate therapies, including allergen avoidance, medications, or immunotherapy (allergy shots). By understanding the allergens triggering symptoms, individuals can take control of their allergies and effectively manage or reduce their symptoms.
| Risks | Challenges | Accuracy |
|---|---|---|
| Slightly swollen, red, itchy bumps | Medications interfering with test results | False-positive and false-negative results |
| Severe allergic reactions (rare) | Skin conditions affecting accuracy | Interpretation based on medical history and symptoms |
Allergy Testing and Treatment Plan
Once allergy test results have been obtained, they play a crucial role in developing an effective treatment plan. By identifying the specific allergens causing symptoms, allergists can recommend appropriate therapies to manage and alleviate allergic reactions. The treatment plan may involve various strategies, including allergen avoidance, medications, or immunotherapy (commonly known as allergy shots).
Allergen avoidance is an essential component of the treatment plan. Based on the identified allergens, individuals can take proactive measures to minimize exposure. For example, if dust mites are the culprit, using hypoallergenic bedding, regularly washing bedding in hot water, and maintaining a clean and dust-free environment can significantly reduce symptoms.
Medications may also be prescribed to manage allergies. Antihistamines, nasal corticosteroids, and decongestants are commonly used to relieve symptoms such as sneezing, itching, nasal congestion, and runny nose. These medications can be taken orally or as nasal sprays, depending on the specific symptoms and severity of the allergies.
| Treatment Options | Description |
|---|---|
| Allergen Avoidance | Minimize exposure to identified allergens through lifestyle changes, environmental modifications, and proper hygiene practices. |
| Medications | Prescribed oral or nasal medications to relieve allergy symptoms, such as antihistamines, nasal corticosteroids, and decongestants. |
| Immunotherapy | Allergy shots containing small amounts of identified allergens to desensitize the immune system and reduce the severity of allergic reactions over time. |
In some cases, allergists may recommend immunotherapy, particularly if allergies are severe or difficult to manage with other treatments. Immunotherapy involves administering allergy shots that contain small amounts of the identified allergen. Over time, this helps desensitize the immune system and reduce the severity of allergic reactions. Immunotherapy is usually recommended for individuals with allergies to insects, pollen, dust mites, or pet dander, and it can provide long-term relief and reduce the need for medications.
It’s important for individuals with allergies to work closely with their allergist to develop a personalized treatment plan that addresses their specific needs. This plan may involve a combination of allergen avoidance, medications, and immunotherapy tailored to the individual’s allergens and symptoms. By following the treatment plan and regularly communicating with their healthcare provider, individuals can effectively manage their allergies and improve their quality of life.
Conclusion
Allergy testing is a vital part of the diagnostic process, helping individuals identify the specific substances that trigger their allergic reactions. Whether through skin tests or blood tests, allergy testing provides valuable insights into the root causes of allergies.
Skin testing, the preferred method, offers high accuracy and cost-effectiveness. By applying allergen extracts to the skin and observing for reactions, healthcare professionals can pinpoint the allergens causing symptoms. Blood tests, on the other hand, are used when skin tests are not feasible or inconclusive.
Medical history and the interpretation of test results are crucial in accurately diagnosing allergies. Allergy testing results guide the development of personalized treatment plans, which may include allergen avoidance, medication, or immunotherapy. With the right management plan, individuals can effectively control their allergies and reduce symptoms, improving their overall quality of life.
FAQ
How does allergy testing work?
Allergy testing involves exposing the skin to suspected allergy-causing substances (allergens) and observing for signs of an allergic reaction. It can confirm whether a particular substance is causing symptoms and help develop an allergy treatment plan.
What are the different allergy testing methods?
Allergy testing can be done using different methods, including skin tests and blood tests. Skin tests involve pricking or scratching the skin with allergen extracts, while blood tests measure IgE antibodies to allergens in the blood.
What is the procedure for skin testing?
Skin testing is performed by applying allergen extracts to the skin and pricking or scratching it to allow the allergen to penetrate. The skin’s response is then observed for signs of an allergic reaction.
How is blood testing for allergies done?
Blood testing involves taking a blood sample and measuring IgE antibodies to specific allergens. The most commonly used blood test is the RAST or ELISA test.
How do I choose the right allergy test?
The choice of test depends on factors such as symptoms, medical history, and specific allergens of interest. Allergists are trained to choose tests that specifically identify the allergens causing the symptoms.
How are allergy test results interpreted?
Allergy test results should be interpreted in conjunction with the patient’s medical history. A positive test indicates the presence of IgE antibodies to a specific allergen, but false-positive and false-negative results can occur.
What role does medical history play in allergy diagnosis?
Medical history provides important information about the patient’s overall health, experiences with possible allergens, and symptoms at different times of the year. It helps establish a connection between allergy test results and allergic disease.
What are the challenges and risks of allergy testing?
The most common side effect of skin testing is slightly swollen, red, itchy bumps. In rare cases, a severe allergic reaction can occur. Medications and certain skin conditions can interfere with test results.
How does allergy testing guide the treatment plan?
Allergy test results identify specific allergens causing symptoms, allowing the allergist to recommend appropriate therapies, including allergen avoidance, medications, or immunotherapy. A personalized treatment plan is developed based on the test results.
What is the importance of allergy testing?
Allergy testing is a diagnostic procedure that helps identify specific allergens causing allergic reactions. It enables individuals to manage their allergies effectively and reduce or eliminate symptoms.

