Edema refers to the swelling caused by the accumulation of fluid in the body’s tissues. It can occur in various parts of the body and has different underlying causes. Understanding the different types of edema and their associated symptoms, causes, and treatments can help individuals and healthcare professionals effectively manage this condition.
Swelling, also known as edema, is a common symptom of various health conditions. It can be caused by factors such as injury, inflammation, medication, pregnancy, infections, and underlying medical conditions. The type of edema depends on the specific location and underlying cause.
In this article, we will explore different types of edema, including peripheral edema, pulmonary edema, cerebral edema, lymphedema, macular edema, pedal edema, pitting edema, and non-pitting edema. We will delve into their specific symptoms, causes, and treatment approaches.
Key Takeaways:
- Edema refers to the accumulation of fluid in the body’s tissues, leading to swelling.
- There are various types of edema, such as peripheral edema, pulmonary edema, cerebral edema, lymphedema, macular edema, pedal edema, pitting edema, and non-pitting edema.
- The symptoms of edema can vary based on the type and location of swelling.
- Causes of edema include injury, inflammation, medication side effects, pregnancy, infections, and underlying medical conditions.
- Treatment for edema focuses on addressing the underlying cause and may involve lifestyle modifications, medications, and surgical interventions.
Peripheral Edema
Peripheral edema is a common type of edema that primarily affects the legs, feet, and ankles, and can also occur in the arms. It is characterized by noticeable swelling in these areas, which can cause discomfort and impact mobility. The swelling is often a result of issues with the circulatory system, lymph nodes, or kidneys.
Conditions such as heart failure, kidney disease, and lymphatic damage can contribute to peripheral edema. When these organs are not functioning properly, fluid can accumulate in the tissues of the legs, feet, ankles, and arms, leading to swelling. Peripheral edema can be a sign of an underlying health problem and should be evaluated by a healthcare professional.
Treatment for peripheral edema focuses on addressing the underlying cause. This may involve managing the underlying condition, such as heart failure or kidney disease. Lifestyle modifications, such as elevating the legs to reduce swelling, and reducing salt intake to decrease fluid retention, may also be recommended. In some cases, diuretic medications may be prescribed to help remove excess fluid from the body.
Symptoms of Peripheral Edema
The symptoms of peripheral edema include swelling in the legs, feet, ankles, and arms. The affected areas may feel tight or appear puffy. The skin over the swollen areas may also appear stretched and shiny. In more severe cases, the swelling may cause discomfort or pain. It is important to seek medical attention if peripheral edema is accompanied by other concerning symptoms, such as shortness of breath or chest pain.
| Common Symptoms of Peripheral Edema |
|---|
| Swelling in the legs, feet, ankles, and arms |
| Tightness or puffiness in the affected areas |
| Stretched and shiny skin over the swollen areas |
| Discomfort or pain in severe cases |
Pulmonary Edema: Fluid in the Lungs
Pulmonary edema is a condition characterized by the accumulation of fluid in the lungs. It can be a result of various underlying causes such as heart failure, damage to the heart valves, or other medical conditions affecting the cardiovascular system. When fluid builds up in the lungs, it can lead to symptoms such as shortness of breath, a fast heartbeat, and a persistent cough accompanied by foamy spittle.
One of the hallmark signs of pulmonary edema is the feeling of suffocation, especially when lying down. This occurs due to the impaired ability of the lungs to adequately exchange oxygen and carbon dioxide. As the condition progresses, the accumulation of fluid in the air sacs of the lungs can interfere with normal breathing and pose a serious threat to health.
“Pulmonary edema can be a life-threatening condition if left untreated. Immediate medical attention is crucial for proper diagnosis and prompt treatment.”
It is important to note that pulmonary edema should not be ignored, as it can be a life-threatening condition if left untreated. Immediate medical attention is crucial for proper diagnosis and prompt treatment. The healthcare provider may perform various tests, such as chest X-rays, blood tests, and echocardiograms, to assess the severity and underlying cause of pulmonary edema in order to develop an appropriate treatment plan.
Treatment for pulmonary edema typically involves addressing the underlying cause and alleviating symptoms. This may include the administration of diuretics to remove excess fluid from the body, supplemental oxygen to improve breathing, and medications to manage any associated heart or lung conditions. Lifestyle changes, such as reducing salt intake and maintaining a healthy weight, may also be recommended to prevent the recurrence of pulmonary edema.
Pulmonary Edema Symptoms:
- Shortness of breath
- Fast heartbeat
- Persistent cough with foamy spittle
- Feeling of suffocation
| Pulmonary Edema Overview | Key Facts |
|---|---|
| Definition | Accumulation of fluid in the air sacs of the lungs |
| Causes | Heart failure, heart valve damage, other cardiovascular conditions |
| Symptoms | Shortness of breath, fast heartbeat, persistent cough with foamy spittle, feeling of suffocation |
| Treatment | Diuretics, supplemental oxygen, medications to manage underlying conditions, lifestyle changes |
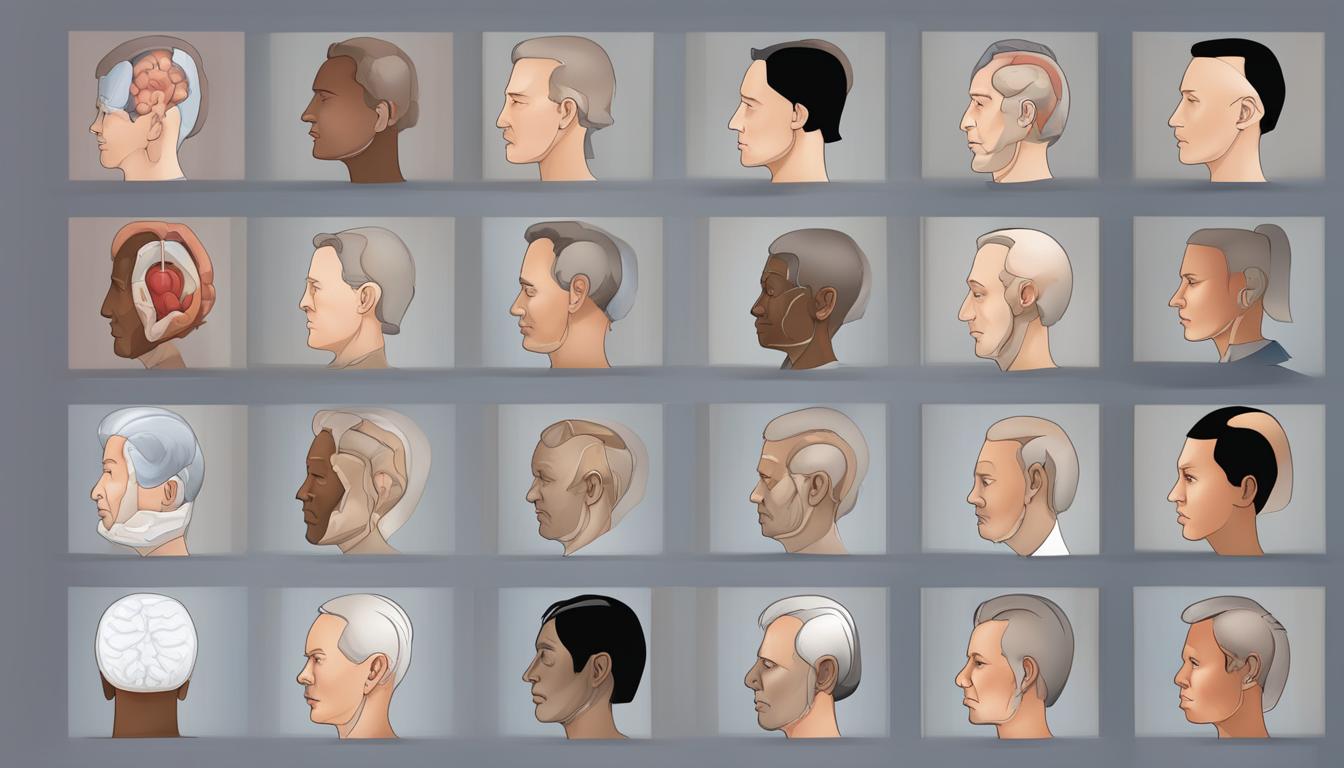
Cerebral Edema
Cerebral edema is a condition characterized by the swelling of the brain due to various factors such as head trauma, blocked blood vessels, allergic reactions, or the presence of a tumor. It is a serious condition that requires immediate medical attention and intervention.
Swelling in the brain can lead to a range of symptoms including headaches, confusion, unconsciousness, and even coma. These symptoms can vary depending on the underlying cause of the cerebral edema.
Head trauma, such as a severe blow to the head, can disrupt normal brain function and lead to the accumulation of fluid in the brain. Similarly, a blocked blood vessel can impede proper blood flow and cause fluid buildup. Allergic reactions and the presence of a tumor can also contribute to cerebral edema.
Due to the potential seriousness of cerebral edema, it is essential to seek prompt medical attention if any symptoms are present. A healthcare professional will perform a thorough evaluation and may order diagnostic tests such as imaging scans to determine the cause and extent of the swelling. Treatment options may include medications to reduce brain swelling, surgical intervention to remove blockages or tumors, or other appropriate measures based on the specific underlying cause.
Lymphedema: Swelling in Arms and Legs
Lymphedema is a condition characterized by swelling in the arms and legs due to fluid buildup. It often occurs as a result of damage to the lymph nodes, which are responsible for filtering germs and waste from the body. Lymphedema can be caused by various factors, with cancer treatments being a common contributor. Surgery and radiation can cause damage to the lymphatic system, leading to the accumulation of fluid.
In the management of lymphedema, it is important to focus on preventing complications and reducing swelling. This can involve a combination of approaches, such as compression therapy, exercise, and skin care. Compression garments help to improve lymphatic flow, while exercise can promote circulation and reduce fluid buildup. Proper skin care is also essential to prevent infections and maintain skin health.
Table: Comparison of Lymphedema Treatment Approaches
| Treatment Approach | Benefits | Considerations |
|---|---|---|
| Compression Therapy | – Improves lymphatic flow – Reduces swelling |
– Requires proper fitting of compression garments – May be uncomfortable for some individuals |
| Exercise | – Enhances circulation – Reduces fluid buildup |
– Should be performed under professional guidance – Tailored to individual capabilities and limitations |
| Skin Care | – Prevents infections – Maintains skin health |
– Requires regular cleaning and moisturizing – Avoidance of cuts and injuries |
It is important for individuals with lymphedema to work closely with healthcare professionals to develop a personalized treatment plan. This may involve a combination of approaches to effectively manage symptoms and improve quality of life. By following a comprehensive treatment approach, individuals with lymphedema can minimize swelling, prevent complications, and maintain overall health and well-being.
Macular Edema: Swelling in the Eye
Macular edema is a condition characterized by the accumulation of fluid in the macula, which is a part of the eye located in the center of the retina. This swelling can affect the central vision, leading to visual disturbances and potential vision loss if left untreated. Macular edema commonly occurs as a result of damaged blood vessels in the retina, which leak fluid into the macula.
The fluid leakage in macular edema can disrupt the normal functioning of the macula, impairing its ability to transmit clear and sharp images to the brain. As a result, individuals with macular edema may experience blurry or distorted vision, difficulty reading, recognizing faces, or performing tasks that require fine detail. It is essential to seek medical attention if any changes or symptoms in vision are noticed, as early diagnosis and treatment are crucial in preserving and optimizing vision.
There are various causes of macular edema, including eye conditions such as diabetic retinopathy, age-related macular degeneration, and retinal vein occlusion. Additionally, inflammation, eye injuries, or the presence of a tumor can also contribute to the development of macular edema. Treatment options for macular edema depend on the underlying cause and may include medications, laser therapy, or surgical interventions to reduce fluid accumulation and promote better vision outcomes.
| Causes of Macular Edema | Symptoms of Macular Edema | Treatment Options |
|---|---|---|
| Diabetic retinopathy | Blurry or distorted vision | Medications |
| Age-related macular degeneration | Difficulty reading or recognizing faces | Laser therapy |
| Retinal vein occlusion | Loss of central vision | Surgical interventions |
If you suspect that you may have macular edema or are experiencing changes in your vision, it is important to consult with an eye care professional for a comprehensive evaluation and appropriate management. Early detection and treatment can help prevent further vision loss and improve overall visual function.
Pedal Edema: Swelling in Feet and Lower Legs
One of the types of edema that commonly affects individuals, especially older individuals and pregnant women, is pedal edema. Pedal edema refers to the accumulation of fluid in the feet and lower legs, leading to swelling and discomfort. This condition can make it difficult to move around and may be accompanied by reduced sensation in the affected areas.
To effectively manage pedal edema, certain lifestyle changes can be implemented. Elevating the legs frequently throughout the day can help reduce swelling by allowing fluid to drain from the legs. Additionally, reducing salt intake in the diet can play a significant role in minimizing fluid retention. It is also important to stay active and engage in regular exercise to promote proper blood circulation.
For pregnant women, mild pedal edema during pregnancy is often considered normal. However, persistent or severe swelling should be discussed with a healthcare professional to rule out any underlying conditions. In some cases, compression stockings or splints may be recommended to alleviate discomfort and prevent further swelling.
Common Causes of Pedal Edema
- Fluid retention due to hormonal changes during pregnancy
- Increased pressure on leg veins from the growing uterus during pregnancy
- Reduced mobility and prolonged sitting or standing
- Impaired circulation due to underlying conditions like heart failure or deep vein thrombosis
- Medications that can cause fluid retention as a side effect
It is important to note that pedal edema can also be a symptom of a more serious underlying condition. If you experience pedal edema along with symptoms such as chest pain, shortness of breath, or severe pain and redness in the affected limb, seek immediate medical attention.
| Causes of Pedal Edema | Prevalence |
|---|---|
| Pregnancy | Common |
| Heart failure | Common |
| Deep vein thrombosis | Common |
| Medications with fluid retention side effects | Common |
| Peripheral artery disease | Less common |
| Liver disease | Less common |
Pitting Edema and Non-Pitting Edema
Edema can be categorized into two types: pitting edema and non-pitting edema. These classifications are based on whether an indentation remains when pressure is applied to the swollen area. Let’s dive deeper into the differences between these two types and how they can help with diagnosis.
Pitting Edema
Pitting edema occurs when pressure on the swollen area leaves an indentation that persists for some time. This type of edema is often associated with fluid retention and can be an indication of underlying health issues. Some common causes of pitting edema include heart failure, liver disease, kidney disease, and certain medications. It is important to note that the severity of pitting can vary, with deeper and longer-lasting indentations indicating more severe edema.
Non-Pitting Edema
In contrast, non-pitting edema does not leave a visible indentation when pressure is applied. This type of edema is typically caused by factors that do not involve excess fluid retention, such as inflammation or lymphatic obstruction. Non-pitting edema can be seen in conditions such as lymphedema, where damaged lymph nodes impair the proper drainage of fluid. Unlike pitting edema, the severity of non-pitting edema is often determined by the degree of swelling rather than the presence of an indentation.
Diagnosing whether edema is pitting or non-pitting can provide valuable information for healthcare professionals in determining the underlying cause of the swelling. Additionally, the presence or absence of pitting can help guide treatment decisions and management strategies. If you experience any symptoms of edema or notice swelling in your body, it is important to consult a healthcare professional for a proper diagnosis and appropriate treatment.
| Pitting Edema | Non-Pitting Edema | |
|---|---|---|
| Appearance | Indents when pressure is applied | No visible indentation |
| Causes | Fluid retention, heart failure, liver disease, kidney disease, certain medications | Inflammation, lymphatic obstruction |
| Severity | Deeper and longer-lasting indentations indicate more severe edema | Severity determined by the degree of swelling |
| Treatment | Address underlying causes, manage fluid retention | Treat underlying conditions, focus on reducing inflammation or improving lymphatic drainage |
Causes of Edema
Edema can have various causes, ranging from medications and allergic reactions to critical illnesses and head trauma. Understanding the underlying factors contributing to edema can help inform effective treatment strategies and preventive measures.
One common cause of edema is the use of certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids. These medications can disrupt the balance of fluids in the body, leading to fluid accumulation in the tissues.
Allergic reactions can also trigger edema. When the body has an allergic response to certain substances, it releases histamines, which can cause blood vessels to leak fluid into the surrounding tissues, resulting in swelling.
Obstruction of flow can be another cause of edema. When the flow of fluid through the lymphatic system or blood vessels is hindered, fluid can accumulate in the affected area. Conditions such as lymphedema, congestive heart failure, and liver disease can cause this obstruction and result in edema.
Other possible causes of edema include critical illnesses, kidney disease, pregnancy, and head trauma. Critical illnesses, such as sepsis or organ failure, can disrupt the body’s fluid balance and lead to edema. Kidney disease affects the body’s ability to remove waste and excess fluid, resulting in fluid retention and swelling. During pregnancy, hormonal changes and the pressure of the growing uterus can cause edema in the legs and ankles. Head trauma can also trigger edema, as it can disrupt the normal flow of fluids in the brain.
Overall, addressing the underlying cause of edema is crucial for effective management and prevention. By identifying and treating the specific factors contributing to edema, healthcare professionals can help alleviate symptoms and improve the quality of life for those affected by this condition.
Symptoms of Edema
Edema is characterized by the accumulation of fluid in the body’s tissues, leading to various symptoms depending on the location and severity of swelling. Understanding these symptoms can help individuals recognize and seek appropriate medical attention. Common symptoms of edema include:
- Swelling: The most noticeable symptom of edema is swelling in the affected area. This can occur in the legs, ankles, feet, arms, or other parts of the body.
- Pain: Edema can cause discomfort and pain in the swollen area. The severity of the pain can vary depending on the underlying cause and the extent of the swelling.
- Difficulty breathing: In the case of pulmonary edema, fluid accumulation in the lungs can lead to difficulty breathing. This symptom is often accompanied by a rapid heartbeat and coughing.
- Weight gain: Edema-related fluid retention can result in weight gain. The weight gain is typically due to the increased fluid volume in the body.
- Coughing: Pulmonary edema can cause persistent coughing. The cough may be productive, producing foamy spittle or even blood in severe cases.
- Skin indentations: Applying pressure to the swollen area can result in the formation of skin indentations or “pitting”. These indentations may persist for some time before returning to normal.
It’s important to note that these symptoms can vary depending on the underlying cause of edema. Seeking medical advice is crucial for an accurate diagnosis and appropriate treatment.
| Symptoms | Associated Conditions |
|---|---|
| Swelling in the affected area | Peripheral edema, lymphedema, macular edema |
| Pain or discomfort | Peripheral edema, cerebral edema |
| Difficulty breathing, rapid heartbeat, coughing | Pulmonary edema |
| Weight gain | Pedal edema, systemic edema |
| Coughing up foamy spittle | Pulmonary edema |
| Skin indentations after applying pressure | Pitting edema |
Edema Treatment
Treating edema involves addressing the underlying cause of fluid accumulation in the body. The specific treatment approach may vary depending on the type of edema and individual patient needs. Here are some common methods used in the treatment of edema:
Allergy Medications
For edema caused by allergic reactions, allergy medications such as antihistamines and corticosteroids may be prescribed. These medications help reduce inflammation and alleviate symptoms associated with allergic edema.
Fluid Drainage
In cases where edema is caused by obstruction of fluid drainage, medical interventions may be necessary. This can involve procedures to remove the blockage or the use of blood thinners to promote proper fluid flow.
Diuretics
Diuretics, commonly known as water pills, are medications that promote the excretion of excess fluid from the body through increased urine production. They are commonly used to treat edema caused by conditions such as heart failure, liver disease, or kidney disease.
Sodium Restriction
Sodium, commonly found in salt, can contribute to fluid retention in the body. Therefore, reducing sodium intake through dietary modifications can help manage edema. Healthcare professionals may recommend a sodium-restricted diet to help reduce fluid accumulation.
It is important to note that the treatment plan for edema should be tailored to the underlying cause and individual patient needs. Consulting with a healthcare professional is essential for proper diagnosis and management of edema.
| Treatment Method | Description |
|---|---|
| Allergy Medications | Prescribed medications, such as antihistamines and corticosteroids, to reduce inflammation and alleviate symptoms associated with allergic edema. |
| Fluid Drainage | Medical interventions to remove obstructions and promote proper fluid flow in cases where edema is caused by obstruction of fluid drainage. |
| Diuretics | Medications that increase urine production and promote the excretion of excess fluid from the body, commonly used to treat edema caused by heart failure, liver disease, or kidney disease. |
| Sodium Restriction | Dietary modifications that involve reducing sodium intake to help manage fluid retention and decrease fluid accumulation in the body. |
Conclusion
Edema is a common condition characterized by the accumulation of fluid in the body’s tissues. It can manifest in various forms, such as peripheral edema, pulmonary edema, cerebral edema, lymphedema, macular edema, pedal edema, pitting edema, and non-pitting edema. Each type of edema has its own set of symptoms, causes, and treatment options.
To effectively manage edema, it is crucial to understand the underlying causes and mechanisms of each type. Prompt medical attention is necessary, especially for severe or rapidly progressing edema. Treatment plans typically involve addressing the root cause, which may include lifestyle modifications, medications, and surgical interventions.
By recognizing the signs and symptoms of edema, healthcare professionals can make accurate diagnoses and develop personalized treatment plans for patients. Additionally, patients should seek medical guidance to receive appropriate care and prevent complications associated with edema.
FAQ
What is edema?
Edema refers to swelling caused by the accumulation of fluid in the body’s tissues.
What are the different types of edema?
There are various types of edema that can occur, including peripheral edema, pulmonary edema, cerebral edema, lymphedema, macular edema, pedal edema, pitting edema, and non-pitting edema.
What causes peripheral edema?
Peripheral edema is often a sign of issues with the circulatory system, lymph nodes, or kidneys. It can be caused by conditions such as heart failure, kidney disease, and lymphatic damage.
What are the symptoms of pulmonary edema?
Common symptoms of pulmonary edema include shortness of breath, a fast heartbeat, coughing up foamy spittle, and a feeling of suffocation.
What can cause cerebral edema?
Cerebral edema can be caused by head trauma, a blocked blood vessel, an allergic reaction, or the presence of a tumor.
What is lymphedema?
Lymphedema is characterized by swelling in the arms and legs, often caused by damage to the lymph nodes. Cancer treatments such as surgery and radiation can contribute to lymphedema.
What is macular edema?
Macular edema involves the accumulation of fluid in the macula, a part of the eye located in the center of the retina. It is often a result of damaged blood vessels in the retina.
What is pedal edema?
Pedal edema refers to the accumulation of fluid in the feet and lower legs. It is more common in older individuals and pregnant women.
What is the difference between pitting and non-pitting edema?
Pitting edema results in an indent that remains for a period of time when pressure is applied to the swollen area, while non-pitting edema does not leave a visible indentation.
What can cause edema?
Edema can be caused by factors such as medications, allergic reactions, obstruction of fluid drainage, critical illness, congestive heart failure, liver disease, kidney disease, pregnancy, and head trauma.
What are the symptoms of edema?
Common symptoms of edema include swelling in the affected area, pain or discomfort, difficulty breathing, weight gain, persistent coughing, and the presence of skin indentations after applying pressure to the swollen area.
How is edema treated?
Edema treatment focuses on addressing the underlying cause of fluid accumulation and may involve managing allergies with medications, restoring fluid drainage, treating heart failure or liver disease with diuretics, and reducing sodium intake.