Diabetics face a higher risk of losing their limbs due to complications related to their condition. Understanding the causes and risk factors behind limb amputations is crucial for managing diabetes effectively and preventing further complications.
Key Takeaways:
- Diabetes increases the risk of limb amputations due to factors such as high blood sugar levels, smoking, nerve damage in the feet, foot deformities, and poor blood circulation.
- Peripheral arterial disease (PAD) and diabetic neuropathy are common conditions that contribute to limb amputations in diabetics.
- Factors such as a history of foot ulcers, foot deformities, vision problems, kidney disease, and poor blood circulation increase the risk of limb amputations in diabetics.
- Proper foot care, including daily inspection, washing, and avoiding walking barefoot, is essential for preventing foot ulcers in diabetics.
- Recognizing the signs and symptoms of foot and leg problems, such as foot ulcers, enables early detection and prompt medical intervention.
Causes of Amputation in Diabetics
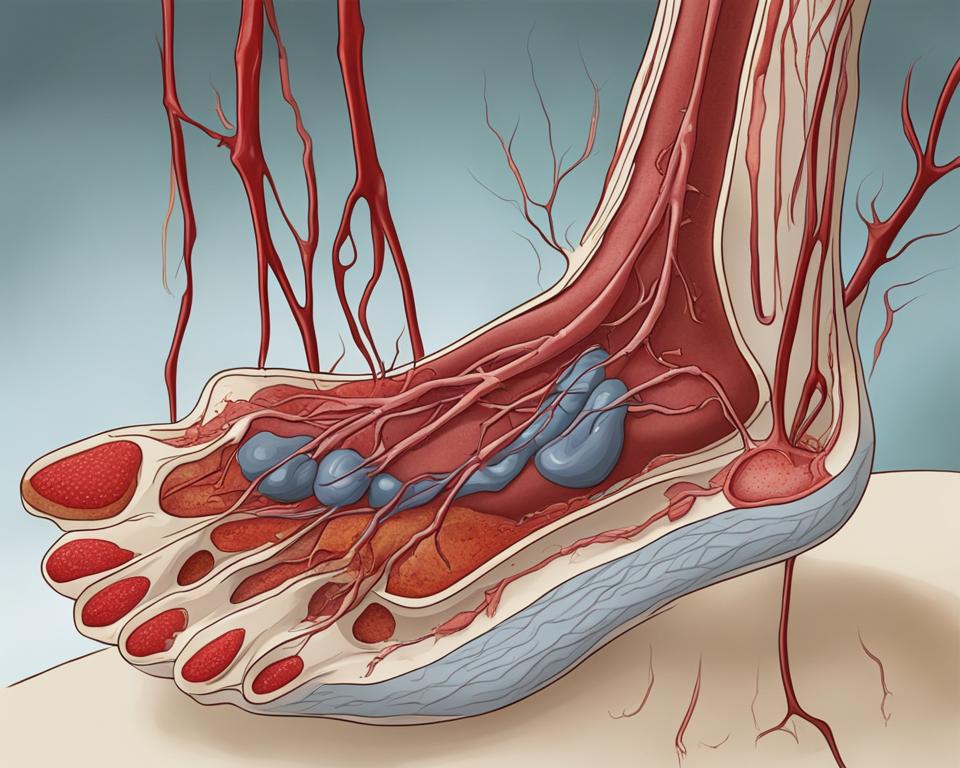
Diabetic individuals are more likely to experience limb amputations due to two common conditions: peripheral arterial disease (PAD) and diabetic neuropathy. PAD causes narrowing of the arteries that supply blood to the legs and feet, leading to ulcers and slow healing. Diabetic neuropathy, a nerve damage condition caused by high blood sugar levels, can result in a loss of sensation in the feet, making it difficult to detect injuries or infections that can lead to amputation.
According to studies and medical research, peripheral arterial disease (PAD) is one of the primary contributors to limb amputations in diabetics. The condition occurs when fatty deposits, known as plaque, build up in the arteries, restricting blood flow to the extremities. Reduced blood flow can lead to tissue damage and the formation of ulcers. Without proper treatment and management, these ulcers can become infected and progress to the point where amputation becomes necessary.
Diabetic neuropathy is another significant cause of limb amputations in diabetic patients. This condition affects the nerves, impairing sensation in the feet and legs. As a result, individuals may be unaware of injuries, infections, or ulcers developing on their feet. Delayed or ineffective treatment can allow these wounds to worsen, leading to serious complications and ultimately, the need for amputation.
Peripheral Arterial Disease (PAD)
| Cause | Symptoms | Treatment |
|---|---|---|
| Plaque buildup in the arteries | Pain, cramping, numbness, ulcers, poor wound healing | Medication, lifestyle changes, angioplasty, bypass surgery |
Diabetic Neuropathy
| Cause | Symptoms | Treatment |
|---|---|---|
| Nerve damage due to high blood sugar levels | Loss of sensation, tingling, pain, increased risk of injuries and infections | Blood sugar control, pain management, foot care, medication |
It is important for individuals with diabetes to be aware of these underlying causes and take proactive measures to prevent complications. Regular check-ups, proper foot care, and effective diabetes management can significantly reduce the risk of amputation and improve overall quality of life.
Risk Factors for Amputation in Diabetes
Diabetes can increase the risk of limb amputations, and several factors contribute to this heightened risk. Understanding these risk factors is crucial for individuals with diabetes to take proactive steps in preventing complications and preserving their quality of life.
Foot Deformities in Diabetes
One significant risk factor for limb amputations in diabetes is the presence of foot deformities. Conditions such as bunions, hammertoes, and Charcot foot can lead to abnormal pressure points and ulcers, increasing the likelihood of infection and tissue damage. Regular foot examinations and proper footwear can help identify and manage foot deformities, reducing the risk of amputation.
History of Foot Ulcers
Individuals with a history of foot ulcers are at a higher risk of limb loss. Foot ulcers in diabetes often result from poor wound healing and compromised blood flow to the extremities. Proper foot care, regular check-ups, and prompt treatment of any ulcers or infections are essential in preventing the progression to amputation.
Vision Problems in Diabetics
Diabetes can affect vision, making it difficult for individuals to detect foot injuries or changes in their feet. Vision problems, such as diabetic retinopathy or cataracts, can hinder proper self-care and early intervention. Regular eye examinations and proper management of eye-related complications are crucial in minimizing the risk of amputation.
Kidney Disease and Limb Loss in Diabetes
Kidney disease, a common complication of diabetes, can also contribute to limb loss. Impaired kidney function can result in poor blood circulation and delayed wound healing, increasing the risk of infections and complications. Managing kidney disease through medication, diet, and regular monitoring can help mitigate this risk.
| Risk Factors for Amputation in Diabetes |
|---|
| Foot Deformities in Diabetes |
| History of Foot Ulcers |
| Vision Problems in Diabetics |
| Kidney Disease and Limb Loss in Diabetes |
Preventing Foot Ulcers in Diabetics
Proper foot care is essential for preventing complications such as foot ulcers in diabetics. By following these diabetic foot care guidelines, individuals can reduce the risk of amputation and maintain optimal foot health:
- Inspect your feet daily: Check for any changes in color, swelling, or cuts. If you have difficulty seeing the bottom of your feet, use a mirror or seek assistance from a family member.
- Keep your feet clean and dry: Wash your feet with lukewarm water and mild soap. Gently pat them dry, especially between the toes, as excess moisture can lead to fungal infections.
- Moisturize daily: Apply a diabetic-friendly moisturizer to keep your skin hydrated, but avoid applying it between the toes to prevent moisture buildup.
- Trim toenails carefully: Cut your toenails straight across and file the edges to avoid ingrown nails. If you have difficulty cutting your nails, seek professional assistance.
- Wear proper footwear: Choose shoes that fit well and provide adequate support. Avoid high heels, tight or pointed-toe shoes, and open-toed sandals.
- Avoid walking barefoot: Always wear shoes or slippers to protect your feet from injury. Even at home, make sure to keep your feet covered.
- Manage blood sugar levels: Keep your blood sugar within the target range recommended by your healthcare provider. Regular monitoring and medication adherence are crucial.
- Exercise regularly: Engage in physical activities that promote circulation, such as walking or swimming. Consult with your healthcare provider before starting any exercise routine.
By incorporating these preventive measures into your daily routine, you can take proactive steps to protect your feet and lower limbs from potential complications.
“Proper foot care is crucial for diabetics to prevent foot ulcers and reduce the risk of amputation. By following these guidelines, individuals can maintain good foot health and overall wellness.”
– Dr. Sarah Thompson, Podiatrist
Table: Common Foot Problems in Diabetics
| Foot Problem | Symptoms |
|---|---|
| Foot ulcers | Open sores, blisters, redness, swelling, pain |
| Peripheral arterial disease (PAD) | Decreased blood flow, slow healing, cold feet |
| Neuropathy | Numbness, tingling, loss of sensation |
| Fungal infections | Itching, scaling, cracking, peeling skin |
| Ingrown toenails | Pain, redness, swelling, infection |
Remember, early detection and prompt treatment of foot problems are key to preventing complications. If you notice any signs of foot ulcers or other foot-related issues, consult your healthcare provider for assessment and appropriate care.
Signs of Foot and Leg Problems in Diabetics
Diabetics need to be vigilant about monitoring their feet and legs for any signs of complications. Detecting potential problems early can help prevent serious issues such as foot ulcers and limb amputations. Here are some common signs to watch out for:
- Open sores or wounds on the feet or legs
- Blisters that do not heal
- Swelling and redness
- Warmth in a specific area
- Persistent pain or a lack of sensation due to nerve damage
- Discolored skin
- Foul odor
If you notice any of these signs, it’s crucial to take immediate action and contact your healthcare provider. Do not ignore any changes or assume they will go away on their own. Timely intervention is key to prevent further complications.
“Early detection and prompt treatment are vital in preventing diabetic foot ulcers and minimizing the risk of amputation. Diabetics should prioritize regular foot checks and report any concerns to their healthcare team.” – Dr. Sarah Johnson, Podiatrist
In addition to these signs, it’s essential to be aware of the symptoms of foot ulcers, as they can lead to serious complications if left untreated. Symptoms may include:
- Pain or tenderness
- A slow-healing wound
- A deep, crater-like sore
- A foul smell coming from the wound
If you experience any of these symptoms or notice a non-healing wound on your foot, seek medical attention promptly. Early intervention can help prevent infection and reduce the risk of amputation.
| Key Signs of Foot and Leg Problems in Diabetics |
|---|
| Open sores or wounds on the feet or legs |
| Blisters that do not heal |
| Swelling and redness |
| Warmth in a specific area |
| Persistent pain or a lack of sensation due to nerve damage |
| Discolored skin |
| Foul odor |
Remember, prevention and early detection are crucial in managing foot and leg complications in diabetics. By staying vigilant and seeking prompt medical attention, you can minimize the risk of serious complications and maintain optimal foot health.
Treatment Options for Foot Ulcers
When it comes to treating foot ulcers in diabetics, early intervention is key. Prompt medical care can prevent complications and minimize the risk of amputation. The treatment options for foot ulcers depend on the severity of the wound and may include:
- Debridement: Removing dead or infected tissue from the ulcer to promote healing.
- Wound cleaning: Thoroughly cleaning the ulcer with a mild antiseptic solution to prevent infection.
- Dressing: Applying an appropriate dressing to the ulcer to protect it from further damage and aid in healing.
- Offloading: Relieving pressure on the affected foot to reduce stress on the ulcer and improve healing.
- Medication: In some cases, antibiotics may be prescribed to treat or prevent infection.
It’s important for individuals with foot ulcers to follow their healthcare provider’s instructions and continue regular monitoring of the wound. Compliance with treatment plans and close communication with healthcare professionals is crucial throughout the healing process.
“Early intervention is key in the treatment of foot ulcers in diabetics. Prompt medical care can prevent complications and minimize the risk of amputation.”
Table: Treatment Options for Foot Ulcers
| Treatment Option | Description |
|---|---|
| Debridement | Removing dead or infected tissue from the ulcer to promote healing. |
| Wound cleaning | Thoroughly cleaning the ulcer with a mild antiseptic solution to prevent infection. |
| Dressing | Applying an appropriate dressing to the ulcer to protect it from further damage and aid in healing. |
| Offloading | Relieving pressure on the affected foot to reduce stress on the ulcer and improve healing. |
| Medication | In some cases, antibiotics may be prescribed to treat or prevent infection. |
By seeking timely treatment and adhering to the recommended care plan, individuals with foot ulcers can increase the chances of successful healing and minimize the risk of complications.
What to Do If Amputation is Necessary
In some cases, amputation may be the only option to address severe tissue loss or life-threatening infections. Amputation procedures aim to remove damaged tissue while preserving as much healthy tissue as possible, allowing for a better chance of successful healing and rehabilitation. If you are faced with the possibility of amputation, it is important to consult with a healthcare professional who specializes in the management of diabetic foot complications.
After an amputation, the road to recovery may involve adapting to prosthetics for improved mobility and independence. Prosthetic devices can help individuals with limb loss regain functionality and engage in daily activities. Rehabilitation programs, including physical and occupational therapy, are crucial in regaining strength, coordination, and adjusting to prosthetics. These programs are tailored to meet each individual’s specific needs, helping them rebuild their lives after amputation.
“Amputation may feel overwhelming, but it is important to remember that there is life after amputation. With the right support, rehabilitation, and proactive self-care, you can achieve a fulfilling and active lifestyle,” says Dr. Emily Johnson, a renowned podiatrist specializing in diabetic foot care.
Living with prosthetics can come with its own set of challenges, but advancements in technology continue to improve the quality and comfort of prosthetic devices. Ongoing follow-up care with healthcare professionals is essential to ensure proper fit and function of prosthetics. These healthcare providers can also offer guidance on how to prevent future complications and maintain optimal foot health.
Table: Tips for Living with Prosthetics After Amputation
| Tip | Description |
|---|---|
| 1 | Follow the guidance of your prosthetist to ensure proper fit, function, and comfort of your prosthetic device. |
| 2 | Engage in regular exercise and physical therapy to build strength and improve mobility with your prosthetic. |
| 3 | Maintain good skin care and hygiene to prevent skin irritation or infections around the prosthetic area. |
| 4 | Take care of the residual limb by keeping it clean and moisturized, following the guidance of your healthcare provider. |
| 5 | Stay connected with support groups and counseling services that specialize in amputee rehabilitation to find emotional support and exchange valuable insights. |
While living with prosthetics after amputation may present initial challenges, many individuals are able to regain their independence and lead fulfilling lives. It is important to remain proactive in self-care, follow the guidance of healthcare professionals, and reach out for support as needed. With determination and the right resources, you can adapt to your new reality and thrive.
Rehabilitation and Support after Amputation
After undergoing amputation due to diabetes-related complications, individuals require comprehensive rehabilitation and support to regain function and adapt to their new circumstances. Rehabilitation programs focus on physical and occupational therapy to help patients rebuild strength, coordination, and independence. Emotional support is also crucial during this challenging time, as individuals may experience feelings of grief, loss, or frustration.
Physical therapy plays a key role in the recovery process by helping patients improve mobility, balance, and endurance. Therapists may use a combination of exercises, assistive devices, and techniques such as gait training to facilitate the transition to walking with a prosthesis or other mobility aids. Occupational therapy focuses on relearning daily activities such as dressing, grooming, and household tasks, ensuring individuals can maintain their independence and quality of life.
Emotional support is vital after amputation, as individuals may face various psychological challenges. Counseling or therapy sessions can help individuals process their emotions, manage stress, and develop coping strategies. Support groups provide a safe space for individuals to connect with others who have undergone similar experiences, fostering a sense of community and understanding. Social workers can assist with practical matters such as accessing resources, financial aid, and long-term care planning.
Table: Rehabilitation and Support Services after Amputation
| Service | Description |
|---|---|
| Physical Therapy | Focuses on improving mobility, strength, and coordination through exercises and assistive devices. |
| Occupational Therapy | Aims to enhance functional independence in daily activities, including dressing, grooming, and household tasks. |
| Counseling/Therapy | Provides emotional support, helps individuals process their emotions, manage stress, and develop coping strategies. |
| Support Groups | Offers a safe space for individuals to connect with others who have undergone similar experiences, fostering a sense of community and understanding. |
| Social Work Services | Assists with practical matters such as accessing resources, financial aid, and long-term care planning. |
Rehabilitation and support services after amputation play a crucial role in helping individuals rebuild their lives and adapt to their new circumstances. By addressing physical, emotional, and practical needs, these services empower individuals to regain function, independence, and overall well-being.
Managing Diabetes to Prevent Further Complications
Preventing complications in diabetes and effectively managing the condition is crucial for individuals who have undergone amputation or are at risk of limb loss. By prioritizing their overall diabetes management, individuals can minimize the risk of further complications and improve their overall health and well-being.
Proper diabetes treatment and foot care play a significant role in preventing complications. It is essential to maintain a healthy diet, engage in regular exercise, and monitor blood sugar levels as prescribed by healthcare providers. Consistently following medication regimens and attending regular check-ups are also important for effective diabetes management.
Additionally, individuals should pay close attention to their feet and practice good foot care habits. This includes inspecting the feet daily, washing them with lukewarm water, and keeping them dry. Avoiding walking barefoot and wearing comfortable shoes that fit well can also help prevent foot ulcers and other complications.
| Preventing Complications in Diabetes | Diabetes Treatment and Foot Care |
|---|---|
|
|
By incorporating these practices into daily life and maintaining a proactive approach to diabetes management, individuals can significantly reduce the risk of further complications and enhance their overall well-being.
Statistics on Limb Loss in Diabetes
Understanding the statistics surrounding limb loss in diabetes is crucial in highlighting the severity of the issue and the importance of prevention and early intervention. These statistics serve as a wake-up call to prioritize foot health and diabetes management.
According to recent studies, a diabetes-related amputation occurs every 30 seconds, underscoring the urgency for effective prevention measures. Between 4-10% of people with diabetes develop foot ulcers, and approximately 5-24% of foot ulcers may lead to amputation within 6-18 months.
This data emphasizes the need for proactive foot care and early detection of complications. By following preventive guidelines and maintaining comprehensive diabetes management, individuals can significantly reduce the risk of limb loss and improve overall health outcomes.
| Statistic | Data |
|---|---|
| Diabetes-related amputations occurring every | 30 seconds |
| Percentage of people with diabetes who develop foot ulcers | 4-10% |
| Foot ulcers that may lead to amputation within 6-18 months | 5-24% |
“The alarming number of diabetes-related amputations highlights the urgent need for proper diabetes management and proactive foot care. By prioritizing regular check-ups, adhering to preventive guidelines, and seeking timely medical intervention, we can reduce the devastating impact of limb loss in individuals with diabetes.”
Importance of Regular Check-ups for Foot Health
Regular check-ups play a crucial role in maintaining foot health for individuals with diabetes. These check-ups allow healthcare providers to monitor and assess any potential issues early, helping to prevent complications and reduce the risk of amputation. During these appointments, healthcare providers, such as podiatrists or endocrinologists, can evaluate nerve damage, circulation problems, and other foot conditions specific to diabetes.
By conducting regular foot check-ups, healthcare providers can detect any signs of foot ulcers, infections, or other foot complications. Early intervention is vital to prevent these issues from progressing and potentially leading to amputation. Additionally, healthcare providers may provide guidance on preventative foot care, including proper hygiene, footwear choices, and overall foot health management strategies specific to diabetes.
Regular foot check-ups are an essential component of comprehensive diabetes care. They complement other aspects of diabetes management, such as monitoring blood sugar levels, following a healthy diet, and taking prescribed medications. By prioritizing these check-ups, individuals with diabetes can proactively address any foot health concerns, significantly reducing the risk of complications and maintaining a high quality of life.
The Benefits of Regular Check-ups for Foot Health
- Early detection and prevention of foot ulcers and other complications
- Evaluation of nerve damage and circulation problems
- Guidance on proper foot care and hygiene
- Individualized management strategies for foot health
- Reduced risk of amputation and other serious foot complications
Quotes from Experts
“Regular check-ups are crucial for individuals with diabetes to ensure the ongoing health and well-being of their feet. By monitoring and addressing any potential issues, healthcare providers can help prevent complications and preserve mobility.”
“Don’t underestimate the importance of regular foot check-ups. They are an essential part of diabetes management and can significantly impact overall foot health.”
Conclusion
Diabetes can lead to serious complications, including limb loss due to conditions like foot ulcers, peripheral artery disease, and neuropathy. However, by prioritizing foot care and diligently managing diabetes, individuals can greatly reduce the risk of amputation and maintain a high quality of life.
Prevention is key when it comes to limb loss in diabetes. Regular check-ups with healthcare providers, such as podiatrists or endocrinologists, are essential for monitoring foot health and detecting any potential issues early on. By addressing concerns promptly, individuals can prevent complications and minimize the need for more drastic interventions.
It’s also crucial to prioritize overall diabetes management, which includes following a healthy diet, engaging in regular exercise, monitoring blood sugar levels, and adhering to prescribed medication regimens. By effectively managing diabetes, individuals can not only reduce the risk of limb loss but also prevent further complications and improve their overall well-being.
In conclusion, taking care of your feet and managing diabetes are essential for preventing complications and limb loss. By remaining proactive and seeking early intervention, individuals with diabetes can significantly reduce the risk of amputation and lead a fulfilling, healthy life.
FAQ
Why do diabetics lose limbs?
Diabetics are at a higher risk of losing limbs due to complications related to their condition, such as peripheral arterial disease (PAD) and diabetic neuropathy. Factors that contribute to limb amputations include high blood sugar levels, smoking, nerve damage in the feet, foot deformities, and poor blood circulation.
What are the causes of amputation in diabetics?
The two common conditions that contribute to limb amputations in diabetics are peripheral arterial disease (PAD) and diabetic neuropathy. PAD causes narrowing of the arteries that supply blood to the legs and feet, leading to ulcers and slow healing. Diabetic neuropathy, a nerve damage condition caused by high blood sugar levels, can result in a loss of sensation in the feet, making it difficult to detect injuries or infections that can lead to amputation.
What are the risk factors for amputation in diabetes?
Certain factors that increase the risk of limb amputations in diabetics include a history of foot ulcers, foot deformities, vision problems, kidney disease, and poor blood circulation. High blood pressure, smoking, and high blood sugar levels also contribute to the risk.
How can foot ulcers be prevented in diabetics?
Proper foot care is essential for preventing complications such as foot ulcers in diabetics. This includes daily inspection of the feet, washing them with lukewarm water, keeping them dry, and avoiding walking barefoot. Good diabetes management, including a healthy diet, regular exercise, and monitoring blood sugar levels, is also crucial in preventing foot ulcers and reducing the risk of amputation.
What are the signs of foot and leg problems in diabetics?
Signs of foot and leg problems in diabetics may include open sores, blisters, swelling, redness, warmth in one area, pain (or lack of sensation due to nerve damage), discolored skin, and foul odor. It’s important to contact a healthcare provider if any of these signs are present or if an ulcer lasts longer than 1 to 2 weeks.
What are the treatment options for foot ulcers?
Treatment for foot ulcers depends on the severity of the wound. Options may include removing dead tissue, keeping the wound clean, and promoting healing. In some cases, antibiotics or surgical interventions such as amputation may be necessary. It’s crucial to seek medical care promptly to prevent complications and minimize the risk of amputation.
What should be done if amputation is necessary?
In some cases, amputation may be the only option to address severe tissue loss or life-threatening infections. The amputation procedure involves removing damaged tissue while preserving as much healthy tissue as possible. Following amputation, individuals may need assistance in adapting to prosthetics and regaining mobility. Ongoing diabetes management and follow-up care are essential to prevent future complications.
What is involved in rehabilitation and support after amputation?
Rehabilitation plays a vital role in the recovery and adjustment process after diabetic amputation. This may involve physical therapy to regain strength and coordination, as well as occupational therapy to improve everyday skills. Mental health support, including counseling and support groups, can help individuals cope with the emotional impact of amputation. Social workers can assist in finding services and planning for long-term care.
How should diabetes be managed to prevent further complications?
Individuals who have undergone amputation or are at risk of amputation due to diabetes should prioritize their overall diabetes management. This includes maintaining a healthy diet, regular exercise, monitoring blood sugar levels, and following prescribed medication regimens. By effectively managing diabetes, individuals can minimize the risk of further complications and improve their overall health and well-being.
What are the statistics on limb loss in diabetes?
Diabetes is a significant contributor to lower limb loss, with statistics showing that a diabetes-related amputation occurs every 30 seconds. Between 4-10% of people with diabetes develop foot ulcers, and approximately 5-24% of foot ulcers may lead to amputation within 6-18 months. These statistics highlight the importance of proactive prevention and effective management of foot and leg complications in diabetics.
Why are regular check-ups for foot health important for diabetics?
Regular foot check-ups are crucial for individuals with diabetes to monitor their foot health and detect any potential issues early. Healthcare providers, such as podiatrists or endocrinologists, can assess nerve damage, circulation problems, and other foot conditions. Routine foot exams, at least once a year or as recommended, play a key role in preventing complications and reducing the risk of amputation.

![Ray Dalio Quotes [Principles, Life, Investment]](https://tagvault.org/wp-content/uploads/2023/04/Screen-Shot-2023-04-19-at-7.57.49-PM.png)